This low cost magnetic resonance imager isn’t [Peter]’s first attempt at medical imaging, and it isn’t his first project for the Hackaday Prize, either. He’s already built a CT scanner using a barium check source and a CCD marketed as a high-energy particle detector. His Hackaday Prize entry last year, an Open Source Science Tricorder with enough sensors to make [Spock] jealous, ended up winning fourth place.
[Peter]’s MRI scanner addresses some of the shortcomings of his Open Source CT scanner. While the CT scanner worked, it was exceptionally slow, taking hours to image a bell pepper. This was mostly due to the sensitivity of his particle detector and how hot a check source he could obtain. Unlike highly radioactive elements, you can just make high strength magnetic fields, making this MRI scanner potentially much more useful than a CT scanner.
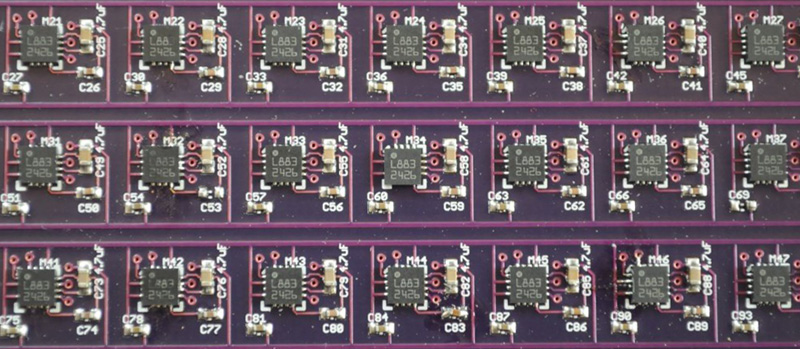
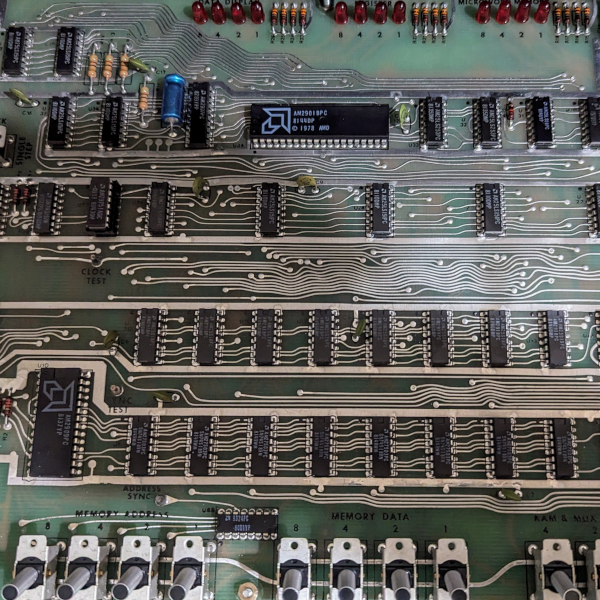
There are a few things that make a low-cost MRI machine possible, the first being a way to visualize magnetic fields. For this, [Peter] is using an array of Honeywell HMC5883L 3-axis magnetometers, the smallest sensors he could find with the largest range. These magnetometers are I2C devices, so with a few multiplexers it’s actually a relatively simple build.
Imaging with these magnetometers is not simple, and it’s going to take a lot of work to make a signal from all the noise this magnetic camera will see. The technique [Peter] will use isn’t that much different from another 2014 Hackaday Prize entry, A Proton Precession Magnetometer. When a proton in your body is exposed to a high strength magnetic field, it will orient towards the high strength field. When the large field is turned off, the proton will orient itself towards the next strongest magnetic field, in this case, the Earth. As a proton orients itself to the Earth’s magnetic field, it oscillates very slightly, and this decaying oscillation is what the magnetic camera actually detects.
With some techniques from one of [Peter]’s publication, these oscillations can be turned into images. It won’t have the same resolution as an MRI machine that fills an entire room, but it will work. Imagine, an MRI device that will sit on a desktop, made out of laser-cut plywood. You can’t have a cooler project than that.















Very Cool!
This man is a god.
MRIs are million dollar machines, if this works it could be a game changer!
They’re also precise in a way that can’t possibly be recreated without using superconducting magnets cooled with liquid helium. Maybe when room temp superconductors become a reality.
Are there compromises that could be made that don’t involve liquid helium but perhaps liquid nitrogen?
I don’t know of any superconducting windings being used at liquid nitrogen temperatures – they’re all in the liquid helium range, with critical temps near single digits Kelvin (ca ~10 K), though it’s an ongoing goal for commercial production. High-intensity windings above superconducting temperatures can be built, but start getting really messy because of the waste heat they generate during operation.
Well if you aren’t putting a person in them commercial examples have existed for a while that don’t need liquid helium to function. Spinsolve is one such brand.
The first nuclear magnetic resonance setups used electromagnets. The field strengths required for small samples is within the realm of “home built” equipment.
The April 1959 Scientific American article “Amateur Scientist” describes a home built nuclear magnetic resonance spectrometer.
https://www.google.com/?gws_rd=ssl#q=Amateur+Scientist+Nuclear+Magnetic+Resonance+
Absolutely. The principle has been demonstrated with permanent magnets and conventional electromagnets. But the modern high resolution devices use liquid helium due to the improved critical current capacity of ReBCO materials, or the field proven performance of the low-temperature superconductors (niobium alloys) where field strengths as high as 10 Tesla are needed for deep tissue imaging. The ReBCO materials are superconducting at liquid nitrogen temperatures, but they are often cooled with liquid helium (usually within a liquid nitrogen jacket) to allow the hundred kilo-ampere currents required to obtain such high magnetic fields.
I have not heard anybody using nitrogen in any modern magnets — a cold head is a better bet, easily allowing the shield temperature to get to 20K and lowering the helium boiloff rate, compared to the 77K you get with nitrogen. Any decent modern magnet will also have a sealed system, recondensing the helium too.
Typical magnets are charged with a current of only a few hundred amps, not a few hundred thousand. I’d hate to see the charging plug for that, not to mention the power supply!
The MgB2 magnets you described in the cold head systems do run in the few hundred amp or less range, and advances in field detection and computational power have made them an excellent tool for imaging.
But the high field systems using the low temperature superconductors Brian described use an inductive charging technique, due to the impracticality of getting many thousands of amps of current through a conventional power cord.
I was referring to conventional NbTi-in-copper-matrix superconductors used in human-scale MRI. Inductively charging a human-scale 3T system sounds like a neat trick. How does that work? Do you have a reference?
But high temp superconductors can’t support multi-tesla magnetic fields.
Fortunately cryogen-free magnets are now available. In these, the cold head usually contains a small amount of helium, but the magnet itself is dry. Sure beats filling a magnet every 3-4 months with a couple of thousand dollars worth of helium, like the old days… It still requires several kilowatts of power (continuous) for the cooling system though — for a measly half watt or so of cooling at 4-5K.
How is it cryogen free if it still requires helium? Is it completely sealed?
No such thing as completely sealed helium. It will escape.
The cold head requires a small (tiny: grams) amount of helium. It’s sealed, but requires service every year or two. The magnet itself is cooled by conduction and is dry. AFAIK, other than a couple of experimental units, commercial human-scale systems don’t operate this way though (these are now usually fill-once and use a helium reliquifier to recover the boiloff).
A recent paper by the University of Rochester says its feasible now. I don’t remember the paper title but it shouldn’t be hard to find.
Here in Canada if you need an MRI for, say cancer, you’ll probably end up in a coffin before you get into an MRI machine, low cost MRI machines like this, even if they are lower resolution than commercial machines, which would be great for pathetic third world health services, like Canada’s. “When a proton in your body is exposed to a high strength magnetic field, it will orient towards the high strength field. When the large field is turned off, the proton will orient itself towards the next strongest magnetic field, in this case, the Earth.” So why isn’t it called a Proton Giggle Camera, that is a much funnier name.
Should be called Nuclear Magnetic Resonance. Just like when it’s used for non-medical purposes. Sadly people are terrified of the word Nuclear so they changed it to MRI.
Funny thing: In a hospital I used to work in, the MRI was in the nuclear medicine department. Across the hall were the SPECT cameras and the technetium cow was a couple of doors over. Another Nuclear scanner would have fit right in.
My local hospital is the same way. They packed all the credit card-wiping and cancer-inducing stuff in the same area. I’d like to think they did it because that way they only need to warn you once.
More likely it is because “medical imaging” is now all lumped together, so X-Ray, CT & nMRI is now all “Radiography”. I had an MRI recently and had a chat with the operator afterwards. The new machine (Kingston Hospital in SW London) has a max field strength of 1.5 Tesla. from her explanation it appears that it is the hysteresis ratio (she didn’t call it that, but it is proportional to Max/Min) that is important. I was having my his scanned (now age 65 and the joints are wearing/worn out), and a region about 40cm long (1.3ft) took about 30mins for 6 different frequencies. She also said that human rated MRI’s are 1 to 1.5 Tesla while industrial rated are between 3 & 7 Tesla. The biggest change in the 20 years she has been operating them is the size of the magnets and the improvement is software for processing and displaying the data. I can certainly confirm the latter, as this is the 6th scan I have had in the last 10 years!
To the OP: most interesting article, and to [Peter] awesome hack.
What? You mean Canada’s medical system isn’t better than what we USED to have in the USA? I’m shocked…
Ok. Sorry for the sarcasm.
I’m the project creator and a Canadian who has been living in the US for over four years. My mother was also diagnosed with very aggressive cancer when I was 12, and several additional cancers in the years following, and so our family has spent a great deal of time in hospitals (she ended up living 18 additional years, passing away last year). I’m also very mildly but chronically ill, which in Canada was never more than a very mild inconvenience, but in the US has become a major and constant medical expense. Having a good deal of experience with both systems, I vastly prefer the Canadian universal health care system, and all other forms of socialized/universal health care. I believe the right to health is a fundamental right of all people, and my first encounter with the US health care system a few months after moving here (and the subsequent heart-attack-inducing bill) was the motivation for most of this, starting with the Open Source CT Scanner.
It is true that the Canadian health care system has genuine issues, like any system. The most well-known of these is that the number of MRIs per capita is about two or three times lower than other countries, and the current government has prioritized lowering taxes superficially rather than increasing health care spending in meaningful ways, like increasing the number of MRIs. The Americans that I talk to who claim universal health care systems have longer wait times than the US system appear unaware that the system is based on triage rather than first-come-first-serve. If someone needs a life saving scan, it’s done immediately, where as scans for elective surgery are done in between high importance scans, as time allows. If someone has a brain tumor, it’s much more important that they’re seen quicker than someone with a knee injury.
In my experience, the wait times of all forms are as long or longer in the US than they are in Canada, but a Wikipedia article on the topic says that they’re about even ( http://en.wikipedia.org/wiki/Comparison_of_the_health_care_systems_in_Canada_and_the_United_States ). I know that my first experience in the ER in the US, I waited so long that I loudly proclaimed (impatient from pain) sometime around hour 6 that I could built a CT scanner in less time than it was taking me to wait for one, when in actuality it took me several times as long to build one.
For me, the most disturbing aspect is that nearly everyone I know here in the US has had or currently has major health issues that remain untreated because they are unable to afford the treatment. Close friends, neighbors, friends of friends. Someone I dated the first year I was here had a broken wrist that had improperly healed because they didn’t seek medical attention, and she was a professor! I have never felt lower or more helpless than when I was turned away from a doctor because of the price of medical treatment, until it happened a second time two years later. I accept that living here will very likely lower my life span because I can’t afford normal regular diagnostic testing, and refuse to spend any more frustratingly endless hours on the phone with sketchy doctors, labs, and “health insurance” companies (what does that even mean??), with kids on the end of a phone reading off a script explaining to me (a doctor) why normal tests or procedures are considered experimental, optional, or some other idiocy. And I also refuse to be one of the approximately 20% of people living in the US who will declare medical bankruptcy sometime in their life. It’s insane. The US stands nearly alone in the developed world as a country without universal health care, and I firmly believe the folks in the US would all be much happier people and many of the social problems here would disappear within a generation were it to join the rest of the developed world and the 60 odd countries worldwide who believe in a fundamental right to health. Had we lived in the US when my mother was diagnosed with cancer, we’d have lost our home shortly after her first treatments and surgeries, I’d have ended up practicing my skills as a waiter professionally sometime around age 15 indefinitely, and the world would be less one doctor of computational neuroscience and science education fueled by numerous designs for open source science tricorders.
I gotta say, I think that’s taking a lot out of context. The debt amounts in each country is different, as is the care, research etc. In the US its not so much they can’t get care, as it is in other countries, is the paying of debt AFTER they got the care. There are 3 major problems that the US has. One is insurance, with insurance there are no caps on the amount a company, person, etc can charge, and someone pays. 2nd is the structure of payment; if a doctor misdiagnoses, or leaves a person untreated, that person still has to pay for services. What services? Nothing was rendered worth value to the customer, so why did they pay for something? 3rd is cronyism; the medical field is balls deep in the government and visa versa, because of that there is near 0 competition in hospitals, research companies, family practice, pharmaceuticals, etc. Its because of people constantly outsourcing their own thinking, and thoughts to other people that most people think doctors are Gods, and make no mistakes, diagnose everything correctly etc. While tons of studies and my own personal experience show doctors are just as human, and prone to the same bias as every other field. If a solution will ever exist, it’ll come when people critically think, therefore never.
I’m the project creator and a Canadian who has been living in the US for over four years. My mother was also diagnosed with very aggressive cancer when I was 12, and several additional cancers in the years following, and so our family has spent a great deal of time in hospitals (she ended up living 18 additional years, passing away last year). I’m also very mildly but chronically ill, which in Canada was never more than a very mild inconvenience, but in the US has become a major and constant medical expense. Having a good deal of experience with both systems, I vastly prefer the Canadian universal health care system, and all other forms of socialized/universal health care. I believe the right to health is a fundamental right of all people, and my first encounter with the US health care system a few months after moving here (and the subsequent heart-attack-inducing bill) was the motivation for most of this, starting with the Open Source CT Scanner.
It is true that the Canadian health care system has genuine issues, like any system. The most well-known of these is that the number of MRIs per capita is about two or three times lower than other countries, and the current government has prioritized lowering taxes superficially rather than increasing health care spending in meaningful ways, like increasing the number of MRIs. The Americans that I talk to who claim universal health care systems have longer wait times than the US system appear unaware that the system is based on triage rather than first-come-first-serve. If someone needs a life saving scan, it’s done immediately, where as scans for elective surgery are done in between high importance scans, as time allows. If someone has a brain tumor, it’s much more important that they’re seen quicker than someone with a knee injury.
In my experience, the wait times of all forms are as long or longer in the US than they are in Canada, but a Wikipedia article on the topic says that they’re about even ( http://en.wikipedia.org/wiki/Comparison_of_the_health_care_systems_in_Canada_and_the_United_States ). I know that my first experience in the ER in the US, I waited so long that I loudly proclaimed (impatient from pain) sometime around hour 6 that I could built a CT scanner in less time than it was taking me to wait for one, when in actuality it took me several times as long to build one.
For me, the most disturbing aspect is that nearly everyone I know here in the US has had or currently has major health issues that remain untreated because they are unable to afford the treatment. Close friends, neighbors, friends of friends. Someone I dated the first year I was here had a broken wrist that had improperly healed because they didn’t seek medical attention, and she was a professor! I have never felt lower or more helpless than when I was turned away from a doctor because of the price of medical treatment, until it happened a second time two years later. I accept that living here will very likely lower my life span because I can’t afford normal regular diagnostic testing, and refuse to spend any more frustratingly endless hours on the phone with sketchy doctors, labs, and “health insurance” companies (what does that even mean??), with kids on the end of a phone reading off a script explaining to me (a doctor) why normal tests or procedures are considered experimental, optional, or some other idiocy. And I also refuse to be one of the approximately 20% of people living in the US who will declare medical bankruptcy sometime in their life. It’s insane. The US stands nearly alone in the developed world as a country without universal health care, and I firmly believe the folks in the US would all be much happier people and many of the social problems here would disappear within a generation were it to join the rest of the developed world and the 60 odd countries worldwide who believe in a fundamental right to health. Had we lived in the US when my mother was diagnosed with cancer, we’d have lost our home shortly after her first treatments and surgeries, I’d have ended up practicing my skills as a waiter professionally sometime around age 15 indefinitely, and the world would be less one doctor of computational neuroscience and science education fueled by numerous designs for open source science tricorders.
Excellent piece Peter. I have lived in the UK for most of my life, and although I have no direct experience of the US health system I have close friends who do.
My own experience over the past decade matches your description of the Canadian system. In 2005 I collapsed while visiting my mother. paramedics arrived within 10 minutes and decided to take me to A&E. They decided I was very anaemic put me on a drip and did blood tests. A consultant came to see me within 4 hours and I was admitted. The next morning I had a colonoscopy and a preliminary diagnosis of bowel Cancer. The next day i had a CT in the morning and an MRI in the afternoon. by the end of the 3rd day the consultant told me I needed surgery, but that I was too week and would need to have a blood transfusion and be “built up”. By the end of the week he gave me a date for the surgery in 3 weeks. I have been clear of cancer for 10 years.
My consultant surgeon, who I still see regularly, also works in the private sector. He says that most surgeon who do both do so because the public sector has all the “interesting” work!
Keep up the good work. And to those who think that the “free market” makes the US system better, and hate on “Obamacare”, shame on you for being blind to the facts.
I am Canadian and do support universal health care but as you said Canada has 2-3 times less MRI machines than other developed countries, which means I assume more than he U.S., so Canada needs your project, please disregard my sarcasm and get back to your work, it’s much more important than responding to me.
We have a vet show in the UK called Supervet and even they have an mri scanner, I think thats kind of crazy when a large percentage of the humans in the world don’t have access to one.
You should move to Portugal! Sure there are a few idiosyncrasies of the Portuguese people but you will find us civil civilized and warm. This country needs and welcomes people that have their hart where you do and a brain like you have, we offer excellent universal health care in return. Low income but not a bad lifestyle!!
I’m glad I live in Australia. MRI’s only cost $100 or so and some people get it for free. So universal health care does work, who’d of guessed…
Canada also gave (billed many thousands of dollars for) the world the Therac 25. https://en.wikipedia.org/wiki/Therac-25 I think they were inspired by classic Star Trek electrical engineering.
“Here in Canada if you need an MRI for, say cancer, you’ll probably end up in a coffin before you get into an MRI machine,”
I heard there is a 10 month waiting list for pre-natal too!
B^)
I love messing with coded aperture imaging, but it comes with a lot of headaches. Why go through the gymnastics of a coded field? As Peter observes, you can’t generate high order codes in magnetic fields, so you’re limited right off the bat. You’d get better SNR with a simple gradient, the coils and drivers would be far simpler, and the reconstruction is a simple FFT.
IIRC, somewhere around the turn of the millennium Steven Wright et al. at TAMU built a fully functional MRI around a bunch of permanent magnets, a ham radio and a PC with some NI cards. All for the price of a decent used car. Creditable images too.
Oddly, Steve Wright is my adviser. You are correct that some work was done in the lab on this and published in 2002. I think this is what you are making reference to http://www.ece.tamu.edu/~mrsl/papers/magma_2002_13(3)_wright.pdf We still have that system around the lab, but really use it. The main difficulties in this type of a setup are exactly what you would expect (if you are familiar with MRI). The field homogeneity is difficult to get good enough to produce high quality images, and the strength of permanent magnets drifts with temperature. Also, the SNR on these low-field systems always proves to be somewhat limiting. We’ve actually put together an undergrad lab class where the students use desk top MR systems that are very similar (again, we built those in house) and have been, slowly, trying to make improvements to the quality and push down the costs. It’s worth pointing out that we use either Fourier encoded images (the normal now) or projection reconstruction images (like CT, somewhat easier for students to execute on).
Also, a few points of interest relevant to other comments: MRI isn’t called NMR, because NMR is the physical phenomenon and more strongly associated with NMR spectroscopy. The use of spatial encoding gradients and narrow band, single nuclei, signal chains strongly differentiate the two techniques. That’s why we call it MRI, and not NMR.
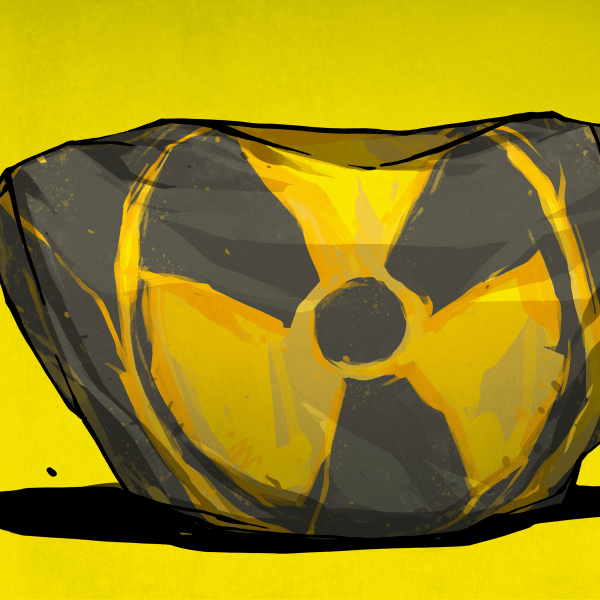
Current gen hospital systems use niobium titanium super conducting magnets with field strengths of either 1.5T or 3T. There are some whole body research systems at 7T, but nothing clinical above 3T. These are all kept in a liquid helium bath and use recondensing cold-heads to recycle the helium. Those things bring their own maintenance nightmares, though.
I’m not clear on why one would use a set of magnetometers to make these measurements. Pre-polarized MRI using resistive magnets and gradient encoding is well described and understood, and can work reasonably well. These magnetometers might give a speed advantage, but it’s not clear that they will provide an SNR that makes them useable sense the signal strength will be so low (follows roughly the square of B0). There are atomic magnetometers that might be more feasible, if a bit trickier to build. Still, not having access to gradients makes it hard to take real advantage of MRI (e.g. contrast developed from things other than proton density, which is the primary advantage of this imaging modality).
Hehe. Nice to hear it’s still going on there. I’m pretty sure I saw the work at an ISMRM conference, probably 2001. The last MR system I used was that cute little 1T Icon (nee Aspect), which did remind me of Wright’s work.
Thanks for the confirmation on the magnet tech too. Recondensing systems had just become commonly available by the time I defected from MRI around ’04.
I remember reading this Wright et al. (2002) paper! I can’t imagine how much work went into piecing together and balancing the magnet from the 300 smaller magnets!
I see where your confusion is. The idea here is to try to put together an inexpensive prepolarizing MRI that also relaxes the constraint on the readout field being homogeneous — so both polarizing and readout field are inhomogeneous. The magnetometer array would be used to characterize the inhomogeneities in the readout and gradient fields, so that spatial information can still be recovered. The article summary suggests that the magnetometer array would be used for signal acquisition, but it’s only used for calibration and characterizing the field, and not involved in the signal acquisition process afterwards. The MRI signals would of course be far to small and fast to measure with the HMC5883L magnetometers.
I remember reading about MIT working on low power (no liquid gas cooling) MRI few years ago, wonder whatever happened to that.
an old book I have:
http://ruemohr.org/~ircjunk/images/340_diymri.gif
who can translate that to semiconductors and post to HaD?
You might at least tell people where that circuit comes from.
It’s from “The Amateur Scientist” by C.L. Strong (page 340) and the text gives a good description of the circuit. It’s a 6.1 MHz fixed oscillator and a plate current amplifier.
The small coil oscillates at 60 Hz, which makes the total magnetic field oscillate above and below the 6.1 MHz resonance point. The plate current of the 6AK5 (amplified by the 6AU6) reflects the amount of RF absorbed by the sample.
It’s a fine demonstration of the MRI effect, but doesn’t actually make an image.
Here’s how MRI works.
You put your sample in a magnetic field and send in some radio waves. The nuclei of specific atoms in the magnetic field absorb the radio waves and re-emit them a bit later. You measure the emitted radio waves and from the 3d map of intensity you can reconstruct the structure of your sample using a modified FFT.
The frequency of absorption/re-emittance is dependent on the magnetic moment of the nuclei, which is fixed based on which nuclei you choose, and the strength of the magnetic field. Stronger fields produce resonance with higher frequency radio waves, which have shorter wavelengths, and hence higher precision.
There is no reason that an MRI can’t be built with non-cryogenic magnets, you simply use lower-strength magnets, a lower RF frequency, and accept lower resolution.
For best results the magnetic field has to be completely uniform. The frequency is very sensitive to magnetic field strength, and slight variations from place to place will produce variations in intensity which mess with the reconstruction algorithms.
So to MRI people you usually have to use large magnets to get a big enough uniform field.
That was state of the art a couple of decades ago, but we’ve since progressed quite a bit with signal processing theory and compute power.
What Peter is doing, if I’m reading his project correctly, is making a map of the field strength variations within the scan volume, and using this to adjust his reconstruction algorithm to compensate. That seems innovative.
He did his post-doc in coded aperture processing, so he’s well-suited to the task. He thinks coded-aperture processing can compensate for the variations in magnetic field.
…and I agree with that assessment.
He doesn’t need to actually build a medical MRI, all he has to do is show “proof of concept”. If he can successfully integrate coded aperture processing with MRI technology, it would be an order-of-magnitude improvement in MRI technology and make medical MRI systems much easier to build.
So… yeah. Good project, high concept, and in the spirit of the 2015 HAD prize.
I hate to be harsh, but this description of MRI is NOT correct. In contrast to other imaging techniques in MRI there is no relationship between wavelength of the radio waves and the image resolution/accuracy. Resolution/accuracy is determined by the strength of the gradient coils, the lower limit of detectable signal and ultimately the diffusion of water (i.e. how far do water molecules travel during the imaging process).
The benefit of higher fields is increased polarization and the benefit of higher frequency is increased sensitivity of Faraday detection. Looking at the opposite end of field strengths, at very low frequencies therefore often alternative detection techniques are considered (i.e. squid detection), though they bring their own problems.
This is a great summary, thank you!
With conventional MRIs, the critical feature that enables one to take images is the extremely uniform field — the field intensity varies by only an extremely small amount over the imaging area. This uniformity (“homogeneity”) is achieved using superconducting magnets. These superconducting magnets also typically have large field strengths, but the field strength isn’t critical to the imaging part — a lower field can produce images, it just increases the time that it takes to sample the image.
This uniformity requirement exists for basically every MRI in use since they were developed in 1977, and because of it, MRIs are incredibly difficult and costly to construct and maintain.
This project is about trying to make a new kind of MRI that can make use of non-uniform (inexpensive, easy) magnetic fields for imaging, by very precisely measuring the imperfections in the magnetic field before hand, and then essentially compensating for them with some fancy signal processing techniques in hardware.
Conceptually this is very similar to something called coded aperture spectroscopy, where you intentionally distort the aperture of a spectrometer in specific (but known) ways, in order to make certain kinds of measurements much faster at the expense of added computation and complexity. One of the differences here is that this distortion (the “code”) is generally designed and fabricated for spectroscopy, but here for the MRI it’ll be the measurement of the imperfections in the magnetic field.
If it ends up working, the benefit would be reducing the cost of building an MRI by several orders of magnitude, and potentially being able to construct a new kind of much smaller desktop MRI. It’s not a free lunch, though, the tradeoffs would be numerous — a long calibration step before use (measuring the magnetic field code), and at least for this low-field version, a much longer measurement time. Medical MRIs are also capable of numerous kinds of incredible scanning techniques in addition to the standard structural images that most people aren’t aware of (for example, mapping blood vessels), where as this would likely only be capable of structural images without adding in much more cleverness.
The idea here is to try to create a proof-of-concept that demonstrates this coded aperture technique over a small imaging volume (like a cubic inch or two) using one of the simpler NMR techniques (the pulsed field proton precession magnetometer). It’s still hard, and there are lots of technical challenges (like creating entirely non-metallic linear stages for the magnetic field scanner in the calibration step), but I don’t think it’s impossibly hard, and if you could do it you’d probably rest easy knowing that you’d helped a lot of people. That being said I’m not an expert in MRI and only really have an avidly interested amateur knowledge combined with a really captivating course I took in graduate school, so we’ll have to see how it goes!
Couldn’t you somehow use two fields with two different frequencies, with one frequency that penetrates the human body a little less than the other (maybe it doesn’t work that way at all?) Then, by measuring both and calculating a difference, you’d get something like what you’re doing with the pre-computed changes in the magnetic field – just that you use a difference measured live at sample-time instead of a pre-computed one that might change.
The whole point of a project like this must be to get people to think.
The more people it reaches tne more people think about it and the more chance of someone comIng up with a novel game changing idea.
Large industry and science can get cought up in using safe known solutions its the tinkerers who come up with the new ideas.
This could inspire someone to come up with a new approach that could make it cheaper and more accesable.
I love the idea and have looked into making a DIY MRI machine myself. There are two issues that you will have to overcome for it to be useful: 1) It is nearly impossible to generate strong enough magnetic fields in a non-superconductor to get detailed imaging. Yes, you *can* pump a huge amount of current through even more windings, but you will hit field saturation quickly and will run into major heat problems. 2) You need a HIGHLY homogeneous magnetic field to, again, get detailed imaging. Aside from the supercooling, the reason these machines are so expensive is because they have several smaller coils, sensors, and sophisticated algorithms to smooth out inconsistencies in the field. Failure to do so will lead to a lot of noise, black/white spots, and a generally useless MRI for medical purposes.
I applaud the effort as I’ve been down that road, but the words “affordable” and “MRI” don’t really go together for good, physics-driven reasons.
Just wanted to add that permanent magnet MR imagers have been around for more than a decade. They use a lower magnetic field but with advances in 3D volumetric data collection and 3D Fourier transforms the lower sensitivity is not such a detriment as one might imagine. About 15 years ago I was part of a team that was selecting an MRI for a veterinary school. Even then, some of the vendors could do real-time proton imaging to aid patient positioning.
I would imagin that vector network analysis and aperture synthesis would be valuable tecniques with multiple receiving antennas. Analogue devices sythesizers are becoming cheap enough for economic construction of these devices.
One of the big problems with using precious metal coins is the expense of assaying them. I’ve wondered if an MRI could be used to determine the precise amount of the precious metal (gold, silver, platinum) in a coin. Gold coins are susceptible to being filled with tungsten, which has nearly identical specific gravity.
Based on my inexperience with MRI and 30 seconds of Google searching, I found out there is quite a bit of information on something called “Low Field” or “Earth’s Field” MRI.
http://en.wikipedia.org/wiki/Low_field_nuclear_magnetic_resonance
http://en.wikipedia.org/wiki/Earth%27s_field_NMR
There’s even an “Earth’s Field MRI Teaching System” called the Terranova-MRI.
http://www.magritek.com/products/terranova/
Everyone here is talking about High Field MRI because that’s what we’re all familiar with. But it’s probably marginally easier to build more sensitive magnetometers than to build multi-Tesla supermagnets,
Just a thought.
Great project ! What type of I2C multiplexers do you use ?
There are hall sensors available for +/- 1000gauss (0.1 T) giving +/- 2.5v but where is this measured ? You see Neo magnets advertised quoting the wieght they will pick up. One advert said it depends on the thickness of the iron bit picked up. So I have no idea how to measure this paramter. But the project is awsome–thank-you Peter.
If we can use a distorted field why not have two magnets opposing this seems to concentrate the field. In any case you are only looking at a single slice of the subject. Move them or the detector along for the next strip.
A very interesting study which uses an external magnetometer to measure fluctuations in the earths magnetic field to set the Lamor frequency.http://www.fmf.uni-lj.si/~stepisnik/obj_clanki/MohoricAllInstruScienceTechn04.pdf
You would be better off using the HMC1051 then you could use for a magnetic AC antenna.
See in this video on fusion innovation at mit https://youtu.be/KkpqA8yG9T4?t=1827
They use special tape to create the superconductors..Is this a possibility for creating a high strength field at a more economical cost?
The guys at MIT have stacked this tape and soldered it to create their magnetic fields..its really cool stuff
Also relevant, about a year ago I invented a material that according to two third parties verifiably superconducts at room temperature, now looking for investors. Pretty sure that it would be fine for an MRI scanner, though lack the ability to do any more with it due to the expense and complexity of making it in wire rather than pellet form.
Its actually very simple and could have been made in 1983 but the condensed matter community won’t admit they got it wrong, cuprates max out at 167K yet simple molecules can superconduct as high as 218K.