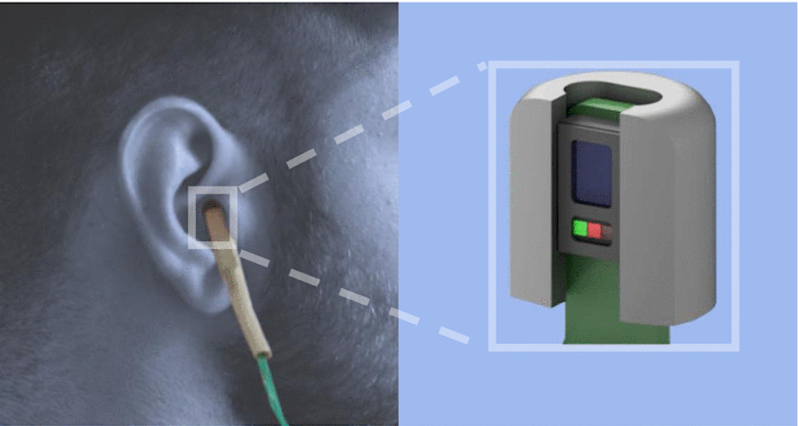
With all the attention given to heart rate monitoring and step counting, respiratory rate monitoring is often overlooked. Smartwatches are starting to incorporate respiratory rate monitoring more and more these days. However, current devices often simply look at breaths per minute without extracting more interesting features of the respiratory waveform which could give us more insight into our bodies than breaths per minute could alone. [Davies] and his team decided they wanted to change that by making an earbud that can measure respiratory rate.
We’ve seen a few commercial earbuds and headphones that can measure heart rate and tune your music to the rhythm of your heart. [Davies’s] project uses photoplethysmography (PPG) which measures changes in blood volume with each heartbeat and is often used to determine heart rate. As it turns out, PPG can also be used to measure respiratory rate as well. When we breathe in, the pressure in our chest cavity decreases which leads to a decrease in central venous pressure and a subsequent decrease in the DC and AC components of the PPG waveform. These modulations in the PPG waveform due to respiration are much slower than the ones we see due to your heart beating, making them often overlooked in common PPG measuring devices. As you could imagine, [Davies’s] project could be really useful for not only determining the respiratory rate, but also examining time domain changes in the respiratory signal that could indicate asthma, sleep apnea, and chronic obstructive pulmonary disease (COPD).
Interestingly enough, he uses similar hardware to extract the PPG signal as we’ve seen in other heart rate monitoring devices. A simple analog front-end with an infrared LED to illuminate blood vessels underneath the skin and a photodiode to measure changes in the LED signal reflected from the tissue underneath the skin. Since the blood volume changes slightly with breathing, the LED signal reflected from the tissue changes slightly as well. And by analyzing these small changes in the reflected LED signal, he could extract the respiratory waveform and look at changes in the signal between people with a respiratory disease like COPD and people without the disease.
We recommend giving [Davies’s] paper a thorough read. Maybe we can incorporate their analysis into other PPG measuring devices we’ve seen here on Hackaday.












There seems to be a formatting problem with the first sentence of the first paragraph.
Has it been tested with various skin tones? Pulse oximeters can give erroneously high readings with darker skin.
Haven’t seen any data regarding the el-cheapo clip on ones, but not surprising that is absolutely not the case with hospital grade devices. They are accurate to a fault except in some extremely uncommon circumstances like CO poisoning and even for that we have multiwavelength co-oximeters.
Hospital quality measures SpCO
https://www.masimo.com/technology/co-oximetry/spco/
Technically correct but you are looking at it wrong. Old oximeter used one or two wavelengths of light. Oxygenated hemoglobin and deoxyhemoglobin absorb at different wavelengths so you can determine the degree of oxygenation. They also measure the absolute magnitude of transmission with each heart beat so that you get a varying waveform and can determine heart rate.
A co-oximeter is an unfortunate name for an instrument that measures multiple wavelengths because some things (again, by coincidence) like carbon monoxide, absorb at yet a different wavelength so with old tech, it looked like your oxygen was “normal” when you were very much not. Another thing is methylene blue, given for… let’s say stuff..it’s a dye and also understandably messes up the “normal” hb absorbtion curves.
The devices you linked are co-oximeters. 99% of the time clinically they are used to simply measure oxygen saturation. I know because I use them all day, every day. You CAN measure carbon monoxide with them but also a bunch of other things.
In any case, the values (any of them) are measured indirectly. You can also take a sample of blood from an artery and measure the partial pressure of many gasses directly, something I also do on a daily basis. But that requires a needle in an artery and people are weird about that for some reason.
I have noticed this too (with a chest strap). The classic waveform seen on an ECG is really the time derivative of the impedance in the chest (dZ/dt), which varies up and down with the breathing. My guess is that this is because the blood vessles being compressed and thus the blood has to move faster to deliver the same volume – remember dZ/dt is reallty the speed of blood moving in and out of the chest. If someone knows if this is correct or if there is another explanation I’m interested to know.
That said, breathing in will oxygenate the blood, which will increase the heart rate. Breathing out will decrease the heart rate to compensate for the lower oxygen contents of the blood – the body runs slower. I think this is a better approch as it becomes less susceptible to noise on the signal. This is because you measure on the instantaneous frequency of the signal instead of the amplitude, and the peaks from beat-to-beat are rather sharp (high SNR). This is even more of a problem with PPGs as they are more smoothed out than ECGs, even if they essentially measure the same thing.
EKG has nothing to do with blood velocity. Or impedance. It is measure the depolarization of the cardiac muscle itself. When the electrical charge of the muscle changes in a coordinated fashion it does so in a direction thus is a vector. Both current and voltage. By convention a deflection away from the reference electrode is “up” and the opposite is true as well. EKG is a plot of this voltage over time directly, is not the derivative.
Breathing oxygenates blood but does not at all change the heart rate due to oxygen content of blood, grossly simplifying. A big breath in, however, lowers the pressure in the chest, sucking blood in (relatively) and this blood has to go somewhere, so your heart pumps out a little more. Blood in has to equal blood out (unless you are shot in the chest. )
Oh also. Control of respiration is a very complex topic but the major driver, under normal circumstances, is partial pressure of CO2 in the blood and, by proxy, pH of the blood. When you put a facemask of oxygen on an otherwise healthy patient, respiratory rate does not change. Even with “more” oxygen in the blood, the amount of CO2 doesn’t change, so respiratory rate remains the same. Again, this is simplified but mostly accurate. There is a reason medical school physiology course is 6 months long and critical care training much, much longer.
I don’t want my smart phone sending my health vitals to Samsung.
That is why I didn’t sign the S-Health app.
If anyone knows how to access older Fitbits without MS Spyware involved, I would like to know.
Do the readings on an oximeters alternate with breaths? If so then combining them with this it could be even more effective.
Readings on pulse-oximeters do not alternate with breaths, the alternate with heart rate. they actually measure the transmission of light through the finger (or whatever it is clipped to) and plot that over time as roughly periodic waveform. On a micro but very measurable level, the diameter of your finger and thus %T changes with pulsatility of blood. however, due to the physics of how you breathe, more blood actually gets pulled into your chest when you breathe in and a bit more pumped out when you exhale. this marco-waveform can (and does) get used to calculate all sorts of other fun, useful physiological parameters.
Hmm, I thought blood oxygenation would change slightly with breaths, thanks for the info.
I’d be quite interested to see how reliable it is while moving. If I even lift a cup of coffee to my face, my Garmin refuses to register a pulse ox reading because I’m moving. It continues to read respiration but I expect partly because I can’t see the averaging that goes on behind. If the intent is to extract breathing waveform, not just rate, I can see that being challenging. Maybe I should read the link, rather than just the HAD post.
There are some interesting (dys)rhythms in breath that are indicative of psychosocial issues as well. I cannot recall the researcher but I know of one scholar in the mindfulness field who pays equal attention to respiratory sinus arrhythmia ask a risk factor for mood disorders. For people with alexithymia or diminished awareness of their mood states, this could possible help them know when they’re upset and learn to identify the sensations associated with that.