As the most important muscle in our body, any serious issues with our heart are considered critical and reason for replacement with a donor heart. Unfortunately donor hearts are rather rare, making alternatives absolutely necessary, or at the very least a way to coax the old heart along for longer. A new method here seems to be literally patching up a patient’s heart with healthy heart tissue, per the first human study results by [Ahmad-Fawad Jebran] et al. as published in Nature (as well as a partially paywalled accompanying article).
Currently, simple artificial hearts are a popular bridging method, which provide a patient with effectively a supporting pump. This new method is more refined, in that it uses induced pluripotent stem cells (iPS) from an existing hiPSC cell line (TC1133) which are then coaxed into forming cardiomyocytes and stromal cells, effectively engineered heart muscle (EHM). After first testing this procedure on rhesus macaque monkeys, a human trial was started involving a 46-year old woman with heart failure after a heart attack a few years prior.
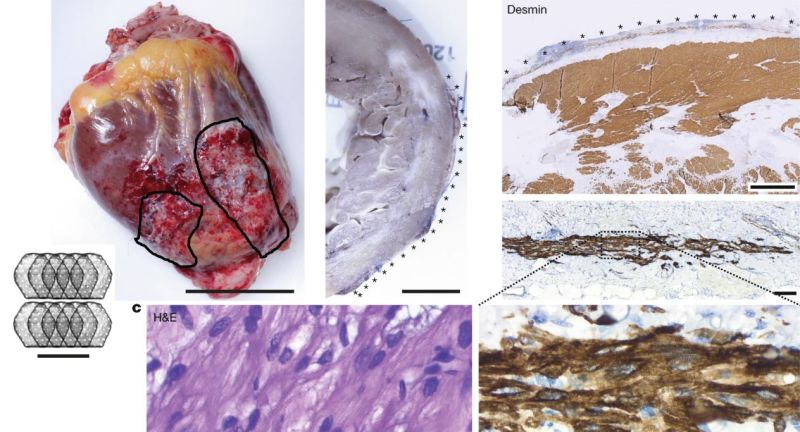
During an operation in 2021, 10 patches of EHMs containing about 400 million cells each were grafted onto the failing heart. When this patient received a donor heart three months later, the removed old heart was examined and the newly grafted sections found to be healthy, including the development of blood vessels.
Although currently purely intended to be a way to keep people alive until they can get a donor heart, this research opens the tantalizing possibility of repairing a patient’s heart using their own cells, which would be significantly easier than growing (or bioprinting) an entire heart from scratch, while providing the benefit of such tissue patches grown from one’s own iPS cells not evoking an immune response and thus mitigating the need for life-long immune system suppressant drugs.
Featured image: Explanted heart obtained 3 months after EHM implantation, showing the healthy grafts. (Credit: Jebran et al., 2025, Nature)













“As the most important muscle in our body, any issues with our heart are considered critical and reason for replacement with a donor heart.”
How about “some issues with the heart”
There are many, many cardiac pathologies that are effectively treated with medication, endovascular interventions, and surgeries that do not put someone on a transplant list.
.
Similarly, “simple artificial hearts…” first there is not anything simple about them. Second, while they may be a bridge to transplant for some people, they are destination therapy for others. And a few other things too…
Finally before I quit, it appears they had to immune suppress which is anything but benign. I can’t quote it exactly became it is 37 pages of solid 6pt font but they had to for the monkeys. You need to do that anyway for a transplant so maybe that was part of the point who knows.
I this case the cells were taken from a cell line, not the recipient. In “real” use they’d use the recipient’s cells, avoiding the need for immunosupressants.
Strange how things go.
Just last night, there was a documentary on TV about this very process. They showed the hexagonal “heart patches” and explained how 25 of them were placed on the heart.