[Gui Cavalcanti], whose name you might recognize from MegaBots, got on a call with a medical professional in San Francisco and talked about respirators. The question being, can we design and deploy an open source version in time to help people?
Unnerving reports from Italy show that when the virus hits the susceptible population groups the device that becomes the decider between life and death is a ventilator. Unfortunately they are in short supply.
The problem gets tricky when it comes to what kind of respirator is needed CPAP, BIPAP, or Hi-Flo oxygen NIV are all out. These systems aerosolize the virus making it almost guaranteed that anyone around them will get infected.
What we need is a Nasal cannula-based NIV. This system humidifies air, mixes it with oxygen and then pushes a constant stream of it into people’s lungs. If we can design a simple and working system we can give those plans to factories around the globe and get these things made. If the factories fail us, let’s also have a version people can make at home.
If you aren’t sure if a ventilator is something you can work on there are other problems. Can you make algorithms to determine if a person needs a ventilator. Can we recycle n95 masks? Can we make n95 masks at home? Workers also require a negative pressure tent for housing patients. This will be especially useful if we need to build treatment facilities in gyms or office spaces. Lastly if you’re a medical professional, can you train people how to help?
Let’s beat this thing. The ultimate medical hackathon begins.

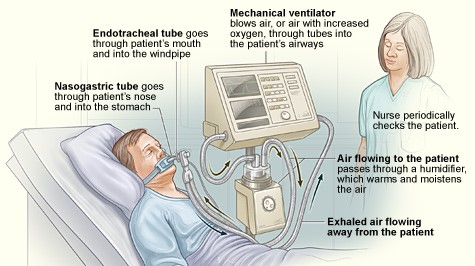












I see a lot of comments about making oxygen. I have been a Registered Respiratory Therapist for the past 28 years. Most hospitals in the USA have a large liquid Oxygen tank on site that feeds the hospitals piped O2. We don’t have an issue with O2 or how to get more. We have an issue with devices to deliver the O2 to a lot of people at once. Mainly Ventilators. We don’t need to reinvent the wheel here, there are companies that already produce plastic disposable vents intended for transport that can be mass produced and deployed that work on a time-cycled, pressure-limited breath. The problem with these vents is that we have no way of monitoring them other than being right next to them. Using them would require a nurse or RT to be at the bedside of every patient on one 24/7. What would most helpful from the hacker community is a device to put in-line with these vents that would provide us with the ability to monitor rate, tidal volume, minute ventilation, and peak pressure. While providing alarms for high and low rate, high and low Tidal volume, high and low peak pressure and high and low PEEP. Having the ability to monitor these things would free up staff to care for more than one pt at a time as we do with existing vents but allow us to be alerted to a pt in need. Do that and you would be a hero to the world!
I see many others creating an actual breathing device. Can you give more info on your thinking? What is the plastic disposable vent? Who is a maker of that existing product? This seems like an easy mod? Why wouldn’t that/those companies build-in the monitoring on their devices? Now that the DHHS has declared liability immunity, I think any company could produce these very rapidly.
glvrrt – I am a physicist and electrical engineer with experience building the kinds of feedback loops and monitoring devices that you’re talking about, although our devices were typically used for things like measuring cooling inflow to some magnetic coils in a cold atom experiment and had nothing to do with medicine. (This is my previous research group at Stanford: https://sites.google.com/stanford.edu/sslab/people/past-members) It would be extremely interesting to hear if I could be useful here, and I would love to learn more about what is required by health professionals on the ground – is there any way we could chat via phone or skype?
– Greg Bentsen
Given the particulars of today’s problems, does it make sense to have a central unit that supports multiple patients?
See our own Bob Baddeley’s marvelous piece on ventilators: https://hackaday.com/2020/03/25/ventilators-101-what-they-do-and-how-they-work/
Short answer: the lung volume, O2 concentrations, and pressure differentials all need to vary across patients, at least when they’re conscious and breathing on their own.
I would suggest looking at the welding industry Oxy/fuel check valves millions of those out there. For air flow and programs
the guy from amigos Dive center (www.amigosdivecenter.com) developed his own cheap easy Nitrox mixer to precisely mix nitrogen and oxygen.
The thing I would be wondering about is how do you find where *specifically* help is needed and moreover that is attuned to your technical skillset? For example, mine is much stronger in computer software, than in designing/engineering mechanisms; and would wonder to what facets of projects related to this that could be used in and more importantly, exactly where things are missing in greater detail.
This is our approach, the YACoVV using water levels to control pressures and camdiscs for timing: https://github.com/auenkind/YACoVV
Old Air Force fight jets all have small oxygen tanks and pilots use face masks to breath this oxygen at high altitudes, just start robbing the equipment, I know the USA has graveyards of old fighter jets, and large aircraft have the drop down masks to use in an emergency (something better than nothing), so start getting aircraft companies to ramp up production of the oxygen system which is already invented, why re-invent the wheel.
Companies that know how to make respirator masks – as opposed to breathing masks – are already doing that.
https://newsroom.resmed.com/news-releases/news-details/2020/ResMed-Statement-on-COVID-19/default.aspx
There is little value having a mask unless you have the machine to drive it and a HCW to monitor it.
Most pf these patients have severely compromised legs, unlike airline passengers who just get oxygen, not ventilation.
A CLOSED system is utmost , we dont need to aerosolize more virus to the environment
we need a pressure driven easy to use system..
Has anyone tried an ambu bag that is compressed by a linear actuator controlled with a timer?
You could also hook up an O2 source and even a sensor to control the mixture. Thinking this could be run by a Pi or just a simple 555timer setup.
Anyone try this? Thoughts?
Like this? https://hackaday.io/project/170507-cosv-cam-open-source-ventilator
Yes! Love it. I was thinking a vertical press instead of the fingers, but this design is better. I’m bookmarking the github and looking forward to the software.
There is an mit project called e-vent pursuing that option
Hi Justin,
Thats very inventive – and I’ve discussed that elsewhere in these threads.
Its very unlikely to work at scale – what we need to focus on is PREVENTING THE SPREAD OF THE DISEASE.
We should redirect our efforts there.
The most important factor is speed to produce, reliability, and least harm. Iron lungs are simple and some have lived with them for as long as 60 years. They are much less complicated. They will save doctors from infection by avoiding intubation! Nurses can put a patient in one. So they free up doctors.
Here’s a video which shows how simple iron lungs are.
https://www.youtube.com/watch?v=xUOlLNKBHiY
“Using two metal barrels and a vacuum cleaner from Sears, he labored just ten hours to develop a crude iron lung. In the following days, Reichart worked with an engineer from Warner Gear to refine the iron lung. Workers at Warner Gear then built a number of the respirators for the hospital.” Reichart distributed the plans for these iron lungs free of charge to anyone who wanted them so, he said, “no other city would get caught without enough of these lifesaving devices.”
https://minnetrista.net/blog/2018/02/20/local-history/jack-reichart-iron-lung/?fbclid=IwAR3osTrWjP4XaIzn7PeKVkPzCihs1q7h40Jbtk0TURY6Subs9Alzf4ricMU
Today easier to cut plastic oil barrels could be used.
An idea – can these clever new ventilator designs that people are producing be used to replace veterinary ventilators? Some veterinary surgeries use ventilator models that can be used on people. These models will already be approved for human use. It would probably be much easier to get approval to use these clever new ventilators for veterinary use. That would free up human-compatible ventilators that are already approved for medical use.
In the UK the Royal College of Veterinary Surgeons is asking vets to donate their compatible ventilators to help with COVID-19:
https://www.bsava.com/News/ArticleID/2704/Government-drive-to-source-ventilator-for-COVID-19-Pandemic-Call-to-action-for-the-veterinary-community
An idea – can any of these brilliant new ventilator designs be used to replace some veterinary ventilators? Some veterinary ventilators are already medically approved for use on people. Getting approval for new designs to be used on people will be slow, but it could be quicker to get approval to use them for veterinary use. Perhaps vets could use these new designs to replace their commercial, human compatible ventilators, donating them to the COVID19 fight?
In the UK, vets are being encouraged to donate any NHS-compatible human ventilators. Could these clever new ventilator designs encourage more vets to donate human compatible ventilators by offering them replacements?
Sorry for duplicate message :( First one didn’t show up for a while so I reposted…
Hi Carl,
A very creative idea …
The main thing is that these devices WERE medically approved for use on people,
but they HAVE been used on animals.
The struggle with this is :-
– getting it past infection control – cannot certify sterility
– scale / training / maintenance etc.
We dont need new designs – perfectly excellent and validated designs are already there.
Production of NEW ventilators has been scaled massively by existing manufacturers – using existing designs with regulatory, technical, maintenance frameworks already in place, and familiar to a trained workforce, with matching consumables, designed for use in hospitals with compatible fittings etc.
Example from ResMed …
https://newsroom.resmed.com/news-releases/news-details/2020/ResMed-Statement-on-COVID-19/default.aspx
I doubt whether repurposing vet ventilators will make much of a dent in the current situation.
In some cases vets are using the identical ventilator models that are already approved for human medical use, and are currently in use in hospitals. So the training and maintenance burden is minimal – they’re already working with the same models. Veterinary operating theatres have to deal with sterility just like we do for humans. Anything that contacts a patient/animal is usually disposable.
This is actually happening in the UK – see link in my post above.
Have developed and low cost PAPR ventilator emergency kit that can be developed at home with basic house hold items with few mechanical components we have developed. The purpose of this kit is to buy some time for patient to breath until medical emergency arrives, which one can make and keep it ready for that emergency situation. our kit is totally mechanical with no batteries or electronic item. but finished idealating it today itself. soon will be posting a brief video about it.
I designed hardware to control any air pump that operates with a brushed DC motor, such as an air mattress pump, which conveniently has a pressure (1psi=70cmh2o) that is reasonably close to what a ventilator can do (tens of cmh2o).
I call it the Ventilificator. The idea is to create a “conversion kit” that converts an air pump into a rudimentary ventilator.
I’m looking for someone to take over the project (firmware, pm, logistics, etc.); I don’t have enough time to do more than hardware.
https://gitlab.com/alex.leblanc/ventilificator/
I am asking ,giving an idea is it poslible to have one big device that could be conected with 10-15-30 patients.
Boris
just an idea
This question is important. Can you tell me if a clean room can be retrofitted to serve as a ventilator? At least for patients needing mild breathing support? The room can be oxygenated and pressurized apart from temperature control. Exhaust air will have to be treated to avoid spread.
Please let me have your thoughts.
on a side note, the necessity for ventilators: endotracheal tubes,
dildo manufacturers are likely very well set up to begin mass producing those items if a mold were to be available.
They already mass produce similarly shaped and used items, they may be able to gain more funding as demands change.
https://www.instructables.com/id/The-Pandemic-Ventilator/
Team, along with two doctors in Seattle, a product design company in Portland, and a university medical device lab, I’m ready to start working TODAY on an open source, mass producible CPAP helmet design. Here’s why this is a win win win:
1) CPAP helmets are proven in europe to keep moderate covid cases out of the ICU, freeing up ventilators for severe cases. Since it’s non-invasive, CPAP helmet therapy can be monitored by nurses. And the oxygen supply (I believe) is a normal bedside or ambulance oxygen supply at 20 cm H20.
2) There is already proven demand for CPAP helmets in the US: Sea Long in Texas makes a device that can be modified for CPAP therapy and they are swamped with orders.
3) We’re not reinventing the wheel, with all the associated risks, JUST making LOTS of a proven device. The helmet is purely mechanical and is relatively
4) I live in northern Italy, so I already have an inside connection to one CPAP helmet manufacturer. My goal is to get a physical model and specs for evaluation, design, prototyping, and testing.
The only issue is that they’re mostly unheard of in the US. I have two friends (an ED doc and anesthesiologist) in Seattle who are FIRED UP about CPAP helmets.
https://it.intersurgical.com/prodotti/critical-care/starmed-castar-up-casco-apribile-per-terapia-cpap
https://www.wsj.com/articles/lacking-ventilators-hospitals-seek-out-alternative-device-11585154579
Use google translate:
http://manualidimedicina.blogspot.com/2017/05/ventilazione-meccanica-non-invasiva.html
See my brand new hackaday on the CPAP helmet:
https://hackaday.io/project/170642-cpap-helmet-non-invasive-ventilation
For what it’s worth, I found this collection of online textbooks around ventilators/ventilation.
Here’s the Patent to one of the Bird Ventilators
https://patentimages.storage.googleapis.com/00/2e/de/b9dcbf0a4068f5/US4044763A.pdf
I believe we should be looking at this as a starting point! no need to reinvent the wheel here!
Hello …..I came to a similar conclusion a little while ago, re. Iron lungs. I found this extremely interesting portable iron lung model made of plywood (!!) but I cannot find information on how is it powered.
It says that some of these devices used vacuum cleaners (!!)
https://en.m.wikipedia.org/wiki/Both_respirator
The story is very basic but it seems to me very exciting.
Question: given the peculiarities of this bug (induces pneumonia) is pure oxygen essential ? Can regular air be of any help, maybe for less critical cases? I am no medical doctor and I am not an engineer.
I should have said Both Portable Cabinet Respirator . It is a “iron lung” type of device but it is not metallic.
Here is a unit being faves in Englandhttps://www.theengineer.co.uk/exovent-covid-19-ventilator/ there is a company in Colorado that was making Nov units and still maintains the FDA certification for it. The first link provides a very good explaination of the advantages. From what I have read, iron kings were once used to ween people off ppv even and they have been used by people at home with no assistance for polio and sleep apnea for decades. Obviously couldn’t do that with a ppv ventilator.
What about Intravenous Oxygen solutions?
Mechanical Ventilation Explained Clearly by MedCram.com https://www.youtube.com/watch?v=6Bdv7QhNNy4
This could be an interesting idea from a very experienced professional
Cheap and nasty but quick ventilators.
The Prime Minister has asked for ideas for a rapid increase in ventilators. Most medical ventilator systems use air pumps and plumbing which is convenient for adding oxygen to the air flow. A possible cheap alternative is to try to replicate the movement of a first aider giving pulmonary resuscitation.
The patient would be lying on their back. Across their chest would be two straps a bit wider than a car seat belt either side of the patient’s nipples. We can use the quick release buckle and length adjustment designed for aircraft seats. There will be plenty available at present! The straps would go round pulleys on each side of the bed and then down at a slope to a spring of chosen extension stiffness. This would be pulled by a crank with chosen throw driven by an electric motor at a chosen rotation speed. DC motors fed from a controlled current source will give a controlled torque and will stall safely. AC motors will run a steady speed depending of supply frequency. Variable frequency converters are now cheaply available.
Based on tests with a weighing machine (and subject to medical advice) I suggest a force of about 40 Newtons would be suitable and a spring length change of about 100 mm. The chest compression movement should be chosen by someone with more medical knowledge than me. All of these could be adjustable, patient by patient.
The system could operate in parallel with more basic oxygen supplies which are available for around £300 . It would need less careful sterilisation between patients.
Possible problems are
Noise disturbance to other patients.
Discomfort, a feeling of being trapped and sleep disturbance.
Requirement for patient to be lying on their backs. There is a report about a higher survival fraction when people lie face down.
Lack of space below modern hospital beds.
Better document available on request.
Cheers
Hi Richard,
That’s an inventive approach …
The things we need to consider are :-
Chest compressions are usually used for patients with cardiac problems (rather than respiratory issues).
Each compressions assists the heart to pump blood around the body. The idea is to compress the heat, rather than the lungs.
Almost invariably, this is accompanied by respiration support, where a first-aider gives the ‘kiss of life’ to provide respiratory support. This pushes air INTO the lungs and EXPANDS the chest.
The iron lung works in a similar way – it expands try CHEST to draw air INTO the lungs.
Compressing the chest will have the opposite effect – to push air OUT of the lungs – which is the opposite of what we need.
We are providing the Latest outbreak of Coronavirus (COVID-19) we have found that the demand for these springs have increased, we are working hard to meet the demand for this particular part in order to aid the production of Ventilators through this difficult time.
https://www.adwin.co.uk/ventilator-springs
Dyson the company that makes vacuum cleaners has developed a ventilator in 10 days and will start producing them for the UK.
Hi there
There is a very advanced Open Source project in Spain, it has already been validated in animals and possibly in a few days it will be available to humans.
https://www.lavozdeasturias.es/noticia/asturias/2020/03/25/asturias-probada-cerdo-forma-exitosa-respirador-3d/00031585127345633606892.htm
https://www.instagram.com/reesistencia_team/
reesistenciateam@gmail.com
First of all, the design has to be extremely simple and robust so anyone
can manufacture or repair it. Think easy to fix Lada vs better Traband, or
the development economist calling for “appropriate technology”. Time cannot
be wasted waiting for a specialist. Also see HBR article ca 1987 about the
IBM Chapel Hill the printer design being simplified for robot so it became
easier to make by hand.
Off pump CABG and asceptic milk came about because power is not relaible
in most of the world. Plus in emergency, power may not be reliable even
here. So diesel seems preferable but a room full of MASH diesel repsirators
would kill faster than COVID. So I’m thinking you have to generate motion
outside the building and transmit it inside. Also it should be at the
opposite end of the building from oxygen concentrators or electrolytic
generators, for smoke and fire reasons. One idea was a pump, with a big
bellows, like induction, powering smaller bellows. The other would be like a
car transmittion shaft running through the building. (Cooney p413 200-400
cc/min, 10-15 pulse/min, also Bronzino 2006 ch 11) I believe you would been
to adjust volume flow and pulse rate by patient, and you need some random
sigh to assure the lungs work right. In the bellows case, I thought maybe to
convolute the pipes into some turbulence, which might however release
projectives, blocked by the inductive discontinuity. Maybe the pumps should
only move the lungs, and to be sure, beter to do the gas exchange through the
blood via canula like dialysis. I cringe at the thought of some third world
kid having to manually pump his granma’s lungs but also wonder why it wasn’t
done in China and italy to those who were triaged against respirators because
of supply. If this goes to the third world manual ventilators need to be
considered. Musk might well provide wonderful batteries but when I was a tee
my uncle-in-law was responsible for the batteries of Greek sub and had
nightmares of them exploding; of course, they too, might be kept at a
distance from patients.
Exacerbating pre-existing medical conditions should also be treated
pharmacologically to minimise respirator time. I was blown away a few weeks
ago at grand rounds that they use colchicine to reduce heart compression from
TB. I’ve used it for gout and it is brutal, but it really works. Maybe it can
reduce lung inflamation. Fibrotic lungs could be treated with relaxin, a
pregnancy antifibrotic hormone which, however, could cause aneurisms.
Further, asma could be treated by rapamycin analogs (DL001 and SAR943).
Another prototype in a very advanced state
https://www.oxygen.protofy.xyz
I’m constantly amazed by people inventiveness ..
There have been many solutions based on the Ambu bag.
Some are better than others, but they all suffer from the same problems …
1. Inability to scale – how can you make 30,000 of these
2. What quality management systems are in place to ensure quality of the end product ?
3. Who will distribute 30,000 of them, and support them in the field ?
4. What happens when the world runs out of ambo bags ?
5. Cycle rate and tidal volume need to be matched to the patient – how will you do that with no feedback controls ?
6. How will you control aerosols – which will infect HCWs, leading to INCREASED fatalities ?
7. What use is it without consumables – lines, masks etc ?
8. How does it respond to patients who breathe spontaneously ?
9.These are needed in ICU’s – it is extremely unlikely any hospital will use it
10. Who will assume legal liability for it when it kills someone ?
I seriously doubt whether AEMPS, FDA, or any regulatory authority ever approve it for clinical use …
and I doubt whether hospital ICU managers or infection control staff will approve using it.
Much better IMHO to stop trying to hack a complex device like a ventilator when companies like Resmed and Medtronic are building certified devices by the tens of thousands, and focus on supporting their supply chains.
I agree with everything you say, but it is not a time for doubt
In some Spanish hospitals triage is being done on which patients are chosen to occupy an ICU unit with a respirator, and in some there are so few ventilators that at 60 years of age they are being left out, ask one of these patients whose life is in danger if you are willing to take the risk.
Many of the risks you point out have been overcome in the approved product.
There is no supplier that can respond to such a high demand for respirators (worldwide), and will preferably cover the demand in your country.
https://www.elconfidencial.com/espana/2020-03-12/respiradores-coronavirus-madrid-compra-comunidades_2492939/
If this has been accomplished in just over a week
https://www.coronavirusmakers.org/index.php/en/53-viseras-entregadas-29-March
why not get the respirators too.
Sorry for my English, it is so bad that I have to rely on google
Hi Thomas,
Thaks for your post.
Yes – Ive mentioned the heartbreaking choices being made in ICUs in some of my previous posts.
Of course, a patient at the point of needing ventilation is not going to be able to answer the question.
And there is a big difference between the patient taking the risk and the care provider taking the risk.
It might answer some of your questions if you take a look at some of my previous posts.
I’m sure the solutions will vary from country to country, because the need varies so greatly.
Thanks also for the links, unfortunately I don’t speak Spanish at all.
Gary – You’ve been very vocal and consistent in this thread. Given your position, do you have a pecuniary interest, one way or another, in any outcome that may or may not be achieved here? The Australian definition of pecuniary interest is fine.
Given Fledge’s focus on the development and commercialization of medial devices, this is a valid question that has not been addressed in any of your posts (which lean towards the advice/input of “stop trying” in regards to ventilators).
Before you take a defense of being/acting offended that someone would ask you such a question: To be clear, I am not saying that you do or you do not have an interest. But it is a valid question given your business and deserving of a clear answer given your position/advice.
Even if you are genuinely offended, the question is deserving of an answer.
Thank you for your participation in this thread. I find this all very interesting and you have brought up some very interesting points.
Hi Cartesia,
Thanks for your question – it’s a perfectly valid one, and I’m not offended at all – and it makes sense to ask it.
No – I have no pecuniary interest in any outcome that might be associated with this thread.
I founded FLEDGE Innovation Labs as a not-for-profit – we exist solely to support MedTech founders, we don’t take a stake in our founder’s projects and they don’t need to sacrifice equity to participate in our programmes. I have no personal stake in this, other than to support our community and to save lives.
I’m not being paid for this work – and I don’t own shares in ventilator companies or anything like that.
We’ve been working on solutions for COVID since early this year when concerns were first raised.
We suspended all our other projects and have been concentrating 100% on our Fight-COVID-19 campaign.
We were in the process of establishing Fledge within one of our local hospitals, that space has been given over for emergency care in case their ICU is overwhelmed.
My family has been engulfed in this in a very personal way. My 91 year-old Mother is a resident in the nursing home where the outbreak in Australia began – her carer and 5 neighbours have died, she was in the first group of people in Australia to be placed in lockdown. I haven’t been able to see her for more than a month. If she catches the virus, the need for ventilation is very highly, so I’m very highly motivated to make sure we ALL have the resources we need, whoever is helped and whatever that takes.
As far as ventilators go, my initial response months ago was to ‘fast-track’ some sort of ‘minimum viable’ ventilator. We looked at Ambu bags very early, but quickly realised that was not a viable solution, for all the reasons mentioned in my previous posts. There are many proposals based on this idea.
We engaged very early with clinicians and respiratory experts to fully understand the problem at a clinical and operation level.
Whatever product is deployed, one of the biggest problems is the control of aerosols (as mentioned the original brief for this thread) which is a lot harder than it sounds, and completely beyond the scope of a DIY solution. If not managed correctly, it will kill more people than it saves.
As recently as yesterday, Ive been told by intensivists they would NEVER let anything like that or any other ‘DIY’ solution into their ICU – where ventilators are most needed. They insist on certified devices.
Another thing I haven’t mentioned before is that you cannot rely on a mains-powered device for every patient. Patients often need to be moved from a MASH tent or field hospital to an ICU – how will they be ventilated in transit ? Resmed’s devices are battery-supported and >robustcertified< ventilators made on quality-managed production lines, with global networks for distribution, training and support. They're ramping up the production of ventilator masks (not respirator masks) by a factor of 10. I've visited their production facility and seen the machines where they make their ventilators and masks. You might like to watch this video from the Resmed CEO :-
https://www.cnbc.com/video/2020/04/01/resmed-talks-ramping-up-ventilator-production-to-combat-covid-19.html#ventilators
Just two days ago, I was a panel member on a discussion to build a ventilator from scratch. This group included the best people in electronics, industrial design, TGA, and medical devices. There is no doubt that these people *could* build a highly-functional and fully certified ventilator from scratch if there was enough time. But others shared my feeling was that it was impossibly difficult in the timeframe, and very unlikely to be approved by regulatory authorities or adopted in ICUs. There were also significant uncertainties about the reliability of supply chains, parts and manufacturing resources, and very little prospect of providing the necessary training, operational support and technical backup in the field.
We can make a much bigger difference by focussing our efforts on supporting existing ventilator manufacturers, for example to prop up their supply chains. We've offered all our expertise and facilities to manufacturers to fabricate parts they're unable to source from their regular suppliers.
Much smarter people than I are advising that we will very likely run out of trained intensivists, beds and consumables like ventilation masks, intubation tubes, and lines long before we run out of ventilators.
Just this morning, our Federal Health Minister said we DO NOT NEED MORE VENTILATORS.
Our Government has been working with existing ventilator manufacturers to bring devices online with what he describes as 'plenty of capacity'. He reiterated my previous point – the limit will very likely be determined by infrastructure, trained people and consumables, not ventilators.
I'm sure its different in other countries because the need varies greatly.
Building a ventilator is one thing – but we need to understand the circumstances within which it will be deployed.
Survival rates are very poor for COVID patients that are fully ventilated.
The question is not 'how can we build a ventilator'.
It should be 'how can we reduce suffering and save lives'.
We need to support supply-chains for companies who know what they're doing and have the resources needed to build and support devices that have the necessary levels of reliability and confidence.
We also need to find better ways to support patients so they DO NOT NEED VENTILATION.
If we can do that, patient treatment will be improved and the demand for ventilators will be reduced, which is much better than making more ventilators.
Thats is where my focus is at the moment.
https://www.youtube.com/watch?v=7vLPefHYWpY&feature=youtu.be
I’m an anaesthetist (in America you’d call me anesthesiologist) and a bit of a geek. Not a ventilator expert but I have a few thousand hours as a user.
I have tried to summarise the key requirements for a truly useful ICU ventilator in a way accessible to non-medical engineers in order to allow the simplest, fastest solution that will actually do the necessary job.
Feedback welcome
https://docs.google.com/document/d/1sdrKYQ0mDOu4bJum6Fx6piRutIJovo7UqFKYHHxUD5A/edit?usp=sharing
Gary – Well said. Thank you for your thoughtful reply. I’ve enjoyed reading your posts.
Thanks Cartesia,
I’m glad you’ve enjoyed reading my posts.
I’d like everyone on this challenge to think again about the design brief …
Making a ventilator – even a simple one – is difficult enough for experts with decades of experience.
Although the objective is noble, IMHO – it is impossible for hobbyists to do this at the necessary speed, quality and scale using parts from a hardware store.
We have tens of thousands of ventilators coming on stream from certified manufacturers.
In Australia, we’ve DOUBLED the number of devices available for COVID patients in the last 4 weeks, and will double that again by the end of April. According to health authorities, there is no need – and no appetite – for home-built solutions.
Clinicians have told me repeatedly – they would never use them.
The approach might be different in other regions, but other factors will come into play that limit the availability and effectiveness of DIY solutions – the difficulties of manufacturing at scale, distribution, deployment, training and support, compounded by looming issues like insufficient numbers of qualified healthcare workers, PPE, beds, O2 supplies, infrastructure and consumables.
It’s easy to neglect issues like regulatory and legal liability – but they are real issues and need to be taken into account.
What will well-meaning hobbyists do when they’re sued because their machine killed someone ?
Focus on ways to KEEP PEOPLE OFF VENTILATORS.
It’s better to have half the number of patients than twice the number of ventilators.
We need to do 4 things :-
1. Help certified manufacturers by supporting their supply chains
2. Stop hoarding masks – our healthcare workers need them
3. If you have N-95 masks at home, donate them to your local hospital
4. Follow the advice of your Health Ministries
– social distancing and hygiene will reduce the load on ICUs and lower the need for ventilators
Ventilators are very complex, and need to take into account a wide variety of complex physiological and biological considerations, like patient’s medical condition, organ failure, pharmacological treatments, comorbidities and so on.
We need to let experts build ventilators.
https://www.independent.co.uk/news/health/coronavirus-iron-lung-nhs-ventilation-papworth-a9440931.html
I am at initial stage in designing mechanical ventilator,the problem i am facing currently is to find the elastic bag around.
Can any one help? I am in Tanzania
Good morning all! I am part of the team developing Ventilate Me/VentilaTM (https://www.facebook.com/VentilaTM) in Timisoara, West Romania.
Wondering if any of you heard about a newly developed OS ventilator being used in a hospital for the treatment of a COVID-19 patient.
Would love to learn what are the doctors’ opinions about their experience working with such a device.
Thanks, good luck in all your efforts!
thank you for inspiring… we made that prototype https://www.youtube.com/watch?v=Ly6TvQ2lU4o
I have an idea to make a small device for hygienical pressing buttons in public places (i. E. Lifts, credit cards terminals). There would be a small stick moved in and out like in a pen. User would Press buttons with it’s tip instead of finger. And each time the tip is inside, IT should be automatically sterilized. There are many available methods:
-chemical (small sponge saturated with i. E. Alcohol)
-heating (the tip could be a resistor)
-discharge (but must be on the whole tip surface)
-ozone generator (the chamber should be closed when hiding the stick)
-UVC LED
Etc.