One of the joys of being a Maker and Hacker is solving problems and filling needs. When you can do both, well, that’s something special. [rodrigo.mejiasz]’s project surely fits into that special category of solving a problem and filling a dire need with his Bedridden Patient Monitor.
While [Rodrigo]’s project page does not specify his motivation for creating this project, one only needs to look as far as their local hospital ward or senior care facility to understand why this device is so wonderful. Healthcare workers and caregivers are stretched paper thin, and their attention is being constantly interrupted.
This is where the Bedridden Patient Monitor comes in. A healthy person can reposition themselves if they are uncomfortable, but bedridden patients cannot. It’s not just that a bedridden patient is unable to get out of bed, but that they are unable to move themselves without assistance. The result is a great amount of pain. And if left unchecked, pressure sores can be the result. These are not only extremely unpleasant, but an added danger to a patients health.
The Bedridden Patient Monitor steps in and provides not just an egg-timer like alert, but helps caregivers track a patients position in bed across even several working shifts. This ensures a continuity of care that might otherwise be easy to miss.
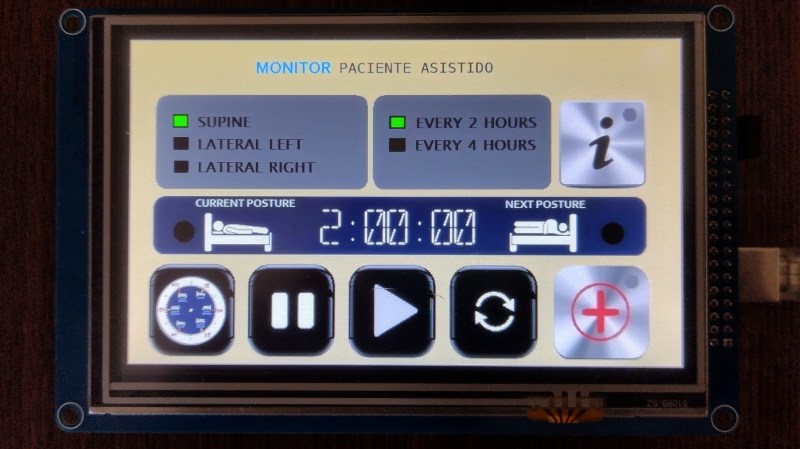
The beauty of this build is in its application but also its simplicity: it’s just an Arduino Mega, a TFT shield with its Micro SD card, and the touch screen itself. A few LED’s and a buzzer take care of alerts. A thoughtfully configured interface makes the devices use obvious so that staff can make immediate use of the monitor.
Makers have a long history diving into the medical field, such as this stab wound treatment device that won the Dyson award in 2021.













Ok, but what if it fails and someone dies?
A lawyer gets richer, a doctor or nurse looses their job and the bean counter who decided they could cut staffing costs gets away scott free.
Oh no, no, no no, no! The bean counter gets a bonus…
check that… no one loses their job.
You no longer have to take care of the bedridden patient. ;)
And when they all go to zero.
He’s dead, Jim.
Decubitus ulcers are no joke. Failure to “turn” patients who cannot do so by themselves can result in untold pain and misery, and costs many millions of dollars annually.
I have special appreciation for this project because I designed a prototype for a device to address this same issue back in the mid 90’s.
http://www.hpfriedrichs.com/medical/px/pr-px.htm
Thirty years ago, you didn’t have the variety of embedded (low power) processors that you do now. There were no MEMS sensors, either–at least nothing I could get my hands on. My prototype used a through-hole PIC processor, some flash ram, a clock crystal, and a couple of mercury switches.
The mercury switches, angled at 45deg, gave you four quadrants of body-position-detection. If I remember correctly, the processor spent most of its time sleeping, but was awakened periodically by an interrupt from a timer disciplined with the 32 kHz clock crystal. This was not only a power saving feature, but provided a real-time clock “tick” for time stamping of data samples.
The use model was to enforce quality control on care personnel. The device was intended to attach to a patient’s clothing or a bra-like garment with anchor loops.The monitor would be removed once a shift, connected to a computer that would download all the collected information, and the data would be archived and analyzed to see if the patient had been rotated according to accepted practice. The software (running on DOS) provided statistics and visual indication of non-compliance.
Since turning a patient can be difficult (it’s certainly easier to rotate a monitor lying on a table instead of rotating the actual patient) the monitor was provided with a tamper switch that could tell if the unit was under tension (on the patient) or not (lying on a table.) Another idea, (not implemented in the prototype) was to monitor temperature, as well. A device in proximity to a patient’s chest likely be warmer than the same device lying on a chair.
I wonder if you could make a bed that tossed patients like a pancake, but gently…
Organ salad.
This is a problem that seems “obvious” to the outsider. How could people forget to turn bedridden patients? Have worked in COVID and other ICU’s for the past two years, and what’s getting overlooked (and often gets overlooked by well-meaning non-medical professionals) is that it’s not that we forget. I know that every two hours during my shift I need to turn my patient. If I don’t turn my patient it’s because I COULDN’T, not because I forgot.
I COULDN’T because I didn’t have enough staff around me to move a 350lb 5’4″ american adequately, or because I was coding someone in another room, or because I was tripled with three patients on ventilators and 5+ drips apiece (drips don’t hang themselves), or because I was helping a coworker catch up from being tripled with three patients on ventilators and 5+drips apiece. Not even to mention the nauseatingly and increasingly giant amount of charting we keep up with on an hourly basis to stay compliant while all this chaos is going on, drawing labs/paging doctors/talking with families/admitting new patients/discharging old patients etc etc etc etc. Oh did I mention this was my 5th shift in a row because without picking up additional shifts we would be tripling more patients every single day? Also I haven’t taken a vacation in a year and a half because our vacation has been cut due to people leaving.
Also, let’s add one more buzzer/light/notification in an environment when alarms are already going off every 10 seconds. We aren’t providing good care at this point in the game, most of us are simply trying to keep your loved one alive until the end of our shift with the hospitals continuing to understaff to near criminal levels to save their profits.
So yeah, cool device, but in the opinion of the guy who going to have to respond to that “turn notification” I don’t need a reminder… I need more staff and I need less work.
Agreed, a buzzer is rarely the problem. Understaffing is. I spent some time in the hospital, and buzzing for help, if it wasn’t an absolute emergency they had other priorities. So, a buzzer among the other annoying noises would just be more irritation.
I developed bedsores twice–being chained down to an IV drip and a catheter with pneumonia limits movement. Bed sores take forever to heal and are so unpleasant, and mine were mild. Serious ones are serious business.
I do think that Covid not only highlighted a shortage of facilities and equipment, but staffing issues and a lack of good management software. I can’t imagine trying to juggle all of that every day (and be nice). Respect.