At the basic level, methods of blood pressure monitoring have slowly changed in the last few decades. While most types of sphygmomanometer still rely on a Velcro cuff placed around the arm, the methodology used in measurement varies. Analog mercury and aneroid types still abound, while digital blood pressure monitors using electrical sensors have become mainstream these days.
Researchers have now developed a new non-invasive method of measurement that does away with the arm cuff entirely. The method relies entirely on video capture with a camera and processing via AI.
Under Pressure
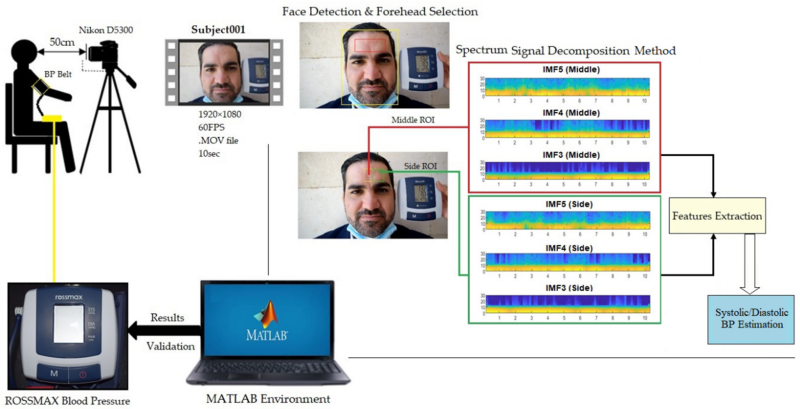
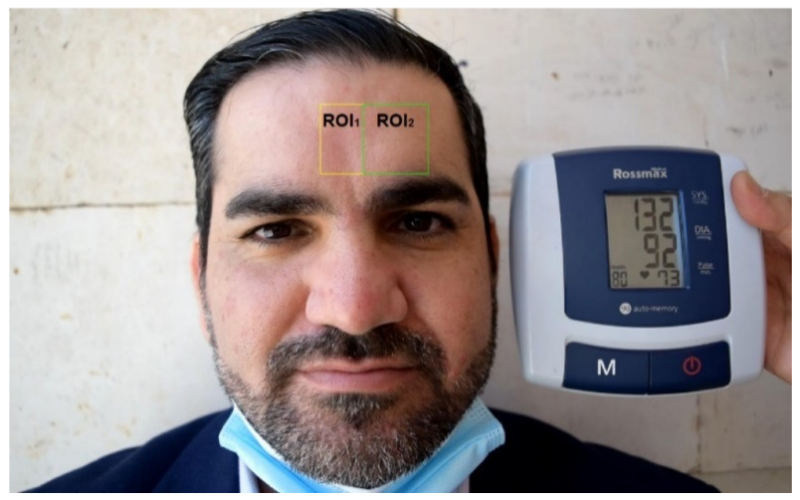
The technique was developed by researchers at the University of South Australia and Middle Technical University, Baghdad. It relies on using a DSLR camera to capture footage of the patient for approximately 10 seconds. The camera is placed a short distance from the patient and is aimed at the face. The video captured is then analyzed by AI to extract indicative signals of cardiac activity from two distinct forehead regions. The system is able to capture both systolic and diastolic blood pressure values as the heart pumps and fills back up.
The system relies on video captured at a resolution of 1920×1080 at 60 fps. Face detection is first used to find the part of the image containing the patient’s head, before zeroing in on the forehead and the precise regions of interest, one in the center of the forehead and a second section off to one side. The forehead region was chosen for analysis as it is least affected by movements from facial expressions, breathing, or blinking. The green channel is used for the analysis as prior research has shown it readily reveals stronger plethysmographic signals – i.e. those corresponding to blood-pressure related volume changes. Analysis of changes to the pixels in the selected analysis regions is fed into a model that estimates the patient’s blood pressure values.
The research builds on earlier work from the same universities, which in 2017 developed a method to determine a person’s heart rate from a video shot via drone. Other work has involved capturing data on blood oxygen levels and respiratory rates. Camera-based techniques have become increasingly common over the past decade, with SIGGRAPH featuring such research regularly over the years.
These methods of measurement have a simple medical benefit, in that they could theoretically reduce the spread of disease that could spread from close contact. The researchers involved in the project cite this as a primary driver of their work, much of which has taken place in the shadow of the coronavirus pandemic.

However, these non-contact methods may give up some accuracy compared to traditional medical practices. In the case of the blood pressure measurement system, testing showed it to be 90% accurate compared to a digital sphygmomanometer. That’s a solid result for a research project, but it means that one in ten patients would be subject to mismeasurement – an unacceptable performance level for medical-grade equipment. It also bears noting that digital sphygmomanometers are not considered the gold-class measurement option. Their measurements use certain base assumptions behind their calculations, and cannot always be relied upon for patients with certain complex conditions. Comparison to a lab-grade mercury sphygmomanometer could provide a truer baseline figure to work from.
The role of AI in medical assessements is a controversial issue, too. Outside of simple measurements, research has also explored the use of AI in performing complex diagnoses using techniques outside the abilities of human perception. The problem is that in many ways, an AI system can be a bit of a black box. Without a proper and comprehensive understanding of exactly what the AI is doing, it’s difficult to trust its measurements or conclusions. In the medical field, this is a major concern, where decisions on treatment regularly come down to life or death.
Technology for the non-contact measurement of vital signs has plenty of useful applications in the medical field. While it’s early days yet, these methods will continue to improve in refinement and reliability in coming years. Expect them to play a complementary role, due to their inherent limitations, rather than replacing traditional methods entirely.













It’s my opinion that taking blood pressure is the *least* scientific practice in modern Western medicine.
The standard deviation is infinite.
The Framingham study, often cited as one of the most robust and well designed and executed studies ever conducted disagrees with your opinion. And so does the entire practice of modern medicine, anti-hypertensive therapy, and so on. As someone who has seen firsthand hypertensive strokes, ruptured aneurysms and also personally treated hypertensive crisis in regular and obstetric patients, I disagree with your opinion as well. Blood pressure is everything. And enormously useful.
Consider your wrist well and truly slapped, Nick!
This schoolmarm-style rhetoric is exactly why people have stopped listening to “experts”. Treat people like adults if you want their respect, otherwise expect to be ignored.
OK pill pusher.
They don’t call them vital signs for nothing. And what does “the standard deviation is infinite” even mean. That’s just crackers.
Maybe Nick needs to elaborate. I mean – he didn’t say “useless” just “least scientific”. Not that I agree but maybe he has a point to consider.
Agreed. Blood pressure measurements are very inaccurate, compared to having a real pressure sensor inside blood veins. Yet these hugely inaccurate results are still valuable enough in modern medicine. That’s why a camera reading can even produce a useful pressure estimation. Craig didn’t read / understand / interpret your statement very well and elaborates on the importance of blood pressure readings I guess.
Ugh. Ok here we go.
The “conventional” method of measuring blood pressure, using a oscillometric method, is both highly repeatable and highly accurate, and highly correlated with invasive blood pressure monitoring in most settings. There will always be fringe cases (see the RN/crit care description below) but please allow me some slack. If repeatable, accurate and precise are not the definition “scientific” I don’t know what is. And I cited a legendary study that correlated blood pressure with a host of negative outcomes, if not established causation (very, very hard to do well) which is also, on a macro level, very, very good science.
I can’t even address the “standard deviation is infinite” even allowing for hyperbole.
There are many, many reasons for a person’s blood pressure to vary for both normal physiological and pathological reasons, but that does not mean that the process of taking a BP measurement is bad. There are standardized techniques for taking a cuff pressure: sitting, relaxed, dominant arm with cuff at the level of the heart. This is standard stuff taught on day 1 of nurse of medical school. Again, the opposite of random, or non-scientific. It is highly standardized for the exact reason that a diagnosis or treatement depends on good numbers. They are not “hugely inaccurate” and confusing the measuring technique with normal (or abnormal) variations in a person’s real BP is a mistake. And the establishment of a hypertension diagnosis, for example, requires repeated measurements over time on multiple occasions. It is not one measurement and you are labeled for life. It is an established trend over time.
Source: practicing MD-PhD academic physician with critical care experience, active research program (not related to BP) in case it matters (it shouldn’t, I’m just a pill pusher).
> the establishment of a hypertension diagnosis, for example, requires repeated measurements over time on multiple occasions. It is not one measurement and you are labeled for life.
You put a person in a stressful social situation, worry them with prospects of illness and death and start measuring their blood pressure. Lo, their blood pressure is elevated, consistently each time you subject them to the same stress. The technical method may be good, but the results can still be garbage and much variable between the people and the circumstances.
All correct. Also a problem that is so common it has the name “whitecoat hypertension.”
For that reason there is probably some value in this actual device in question, mentioned in the article. Repeated and continuous measurements over time, in a non stressful situation as much as being at work in front of a computer is non-stressful.
I will stop commenting on this, as is isn’t productive and I can’t respond to every very valid criticism of modern medicine. I am not every doctor, I’m not the voice of all doctors. And when I attempt to provide explanations, or call out false assumptions or simply incorrect thinking according to contemporary thinking (I am a person, I have biases in a biased speciality full of.. biases) I get ad hominem attacks (not from you), then every caveat, exception and “gotcha” are repeated to me as accusations as though I have anything to do with it.
As always, I thank you for your time to respond to this and many other HaD articles, and enjoy your often technical and insider views about things. It is one of the reasons I still visit this site and comment in the first place, though I may discontinue the latter for the reasons above.
Best
>in a non stressful situation
I get stressed from measuring my blood pressure. I have a phobia about cutting off blood circulation, so the feeling of the cuff alone makes me feel ill.
> I get ad hominem attacks
That’s because you start with the attitude of “Ugh. Ok here we go.”. You started it.
Thank you very much for taking the time to comment in such detail. Some idiots will never be happy so please don’t expend too much effort on them and please know there are plenty of us who are deeply grateful for your service.
To me it looks like you try to imply that some the above commenters are idiots and / or are not grateful for the service of Craig’s service. Can you please elaborate what makes you think that?
“real pressure sensor inside blood veins”
Umm, blood pressure is measuring arterial pressure, inside arteries. Venous pressure is something very different. Both are important but the risks of poking holes in arteries is orders of magnitude higher than poking holes in veins. You only poke holes in arteries when you think there is a significant risk of death or other badness. Veins are punctured routinely for blood tests, IV fluids, etc. Having said that, central venous pressure monitoring is also something you only consider when there is significant risk of death otherwise (because you have to put the catheter just short of the heart.
I check my BP with an automated digital meter every few weeks. It’s usually around 140/90, which is “a bit high.” Eight years ago though I checked and it was 190/120. Checked again the next day, 190/120. After a couple of weeks I realized this was above my pay grade and went to the doctor.
Based on this number I was scheduled for a battery of tests, which my insurance covered. On the stress test my BP went to 240/140 and I started missing heartbeats and throwing PVC’s. On the basis of that I had an angiogram, where it was discovered that I had an 85% blocked LAD artery (aka the Widowmaker). For my 50th birthday I got a spiffy new stent.
If I had not been checking my blood pressure I would be dead.
As they say…opinions are like rectums, Everyone has one. More pointedly, opinions lack any kind of scientific or statistical validation. Buyer beware.
This is very true, but it also applies to your opinion. And mine.
Check the bulges in the forehead, “he’s going to blow”.
I actually havve my own cuff.
On your forehead?
B^)
Bp varies all over the place and the measurements made just minutes ago are much different. So if the camera method is close enough….. do a couple and take the average. It’s a trend that’s important not just one measurement
One wonders if the eye would be a better way of finding out?
I’m a stress case around doctors. Regardless of which of the three home machines I use, my BP always reads consistantly lower than the doctor’s machines. I go by the doctor’s numbers anyway. I’d love a constant monitor. Like the ones that read blood o2 levels. It would be interesting to track.
That is why hospital devices run series of measurements. Even when taking BP nyt yourself start by calming down about five minutes, take measurements on five minutes intervals and average the values. Spot measurement is usefull only for indication. Interesting tech though. I can not fathom where they take the pressure reference, or do they use athmospheric pressure as the imaging is capable of producing the delta only.
I am a retired critical care nurse and Asst. Prof. of Nursing; my passion and teaching revolved around pathophysiology. In the ICU, it’s well known that when the body is in a state of low blood pressure (hypotension), that the physiological response is to save the heart, brain and lungs at the expense of peripheral circulation – extremeties and skin perfusion. So attempting to gauge BP via any method that looks at capillary filling on the surface or extremities is going to have unreliable results, if any at all. Pulse Oximeters suffer from the same issues. Whether a pneumatic cuff (digital or manual), or any other external pressure monitoring device I’m aware of, the measurements are likely of questionable value. In situations where cardiac function and output are compromised invasive sensors (arterial lines for pressures, central venous lines for return oxygenation levels) are used. I question the value of the approach (not the AI, but the attempt to guess at BP by comparing apparent perfusion of two areas of surface skin).
Your bias is showing. To my knowledge, nobody said this was for critical care applications. It would be incredibly useful for long term monitoring of hypertensive people.
Exactly. I check mine with a cuff occasionally, and at the doctor every few months, but I sit in front of a laptop with a camera staring at my face for 50+ hours a week. Even if it’s not the most accurate or precise measurements, it would still be invaluable as a long term monitoring tool.
I agree I am biased, as are virtually all hospital-based providers. Whlie the vast majority of the population never sees the inside of a hospital, let alone a cardiac or medical ICU, our daily experience is “everbody” we deal with as patients is hospitalized, tends to create a mental model that we apply to the rest of the world, incorrectly.
While still teaching I often reminded my nursing students that their view of the world was going to be very, very skewed.
I have an anecdotal basis for my skepticism regarding technology and healthcare which is based on devices I was forced to use, evaluated and purchased by administrators who, in many cases, had not touched a patient in years and were subsequently out of touch with the reality of direct patient care. While the devices were representative of current technological advances, they often provided little real benefit in terms of patient care and positive outcomes. Further, these advances often required attention that was directed away from the patient, resulting in less direct patient contact – typically not conducive to improved patient care.
As to the “incredibly useful for long term monitoring…”, I wonder what the basis for your statement is? Blood pressure is one of the most volatile aspects of our physiology, affected by all manner of external and internal stimuli, and even if provided with the information in the moment, most of us are unable to use that information to control or affect blood pressure.
In similar realm, I have my doubts about the “medical grade” ECG devices being sold to ill-educated consumers – sadly most of the U.S. population. Outside of helping people identify Atrial Fibrillation (often referred to as palpitations) which has some value, the other disrhythmias are frequently life or death medical emergencies, which in many cases result in rendering the victim in no condition to try taking their own ECG – they are unconscious, or worse…
FWIW, I’m not a Luddite regarding tech and medicine (not an accusation you made or inferred). I was a professional software engineer for a couple of major corporations, as well as an independent contractor, for 15 years before I made the career change to Nursing in the early 2000’s. I had both high hopes and expecations for the benefits that tech could/should provide in medicine and healthcare.
However, having taught on-site in multiple hospitals in the San Francisco Bay Area I’ve directly used several systems to provide patient care and chart on patient condition. With one exception, they were stunningly poorly conceived and executed applications when it came to both patient care and user interface design that I ever had the displeasure to be forced to use.
You are rad. Thanks for the measured response. You do a great job of explaining difficult concepts and I hope I’m as good of an educator as you seem to be. I’d love to work with you some day.
Craig, I appreciate the compliment! :)
Are you teaching somewhere? If so, where and what?
As to working together some day – well, I’m fully retired, so, no longer a practicing nurse or teaching nursing. That said, staying in touch would be fun.
I’m now spending my time focused on ceramics/pottery and DIY projects driven by my lifelong (though only recently diagnosed) ADHD, which has resulted in some pretty bizarre, unrelated projects. I’m in the process of reactivating my old youtube channel to reflect what I’m doing now. HAD has taken me on some pretty interesting project wanderings resulting in a lot of stuff learned, as well as more than a couple of rabbit holes! :)
my embarrassing junk email from when I was 15 is elias666 at hotmail etc, reach out I’ll check it and get back to you.
my real ones are just my full name, much to much info for a public forum. cheers
I’ll drop you a note. Look for something from an old alternate gmail acct referencing my nursing background. I understand about not publishing more personal contact info!
This is a world-class response. Everyone is biased. A bias alone isn’t the problem, if it’s relevant to the situation, driven by the predominant details, and has repeatable outcomes better than rolling dice. But, take it out of the situation for which it’s appropriate and it becomes just another means of being wrong with certainty.
The only time bias isn’t at all helpful is when there’s all the time in the world to actually test and measure every possible combination. In minesweeper, the equivalent would be demining by clicking every square; preferentially clicking (or avoiding) certain squares based on knowledge of past outcomes is bias, and the only thing that makes it “good” or “bad”, is “if it consistently beats random choice”.
Having a bias is fine. Having a blind bias without a closed feedback loop is a problem, at least if errors matter. Having a bias, but tracking its long-term performance and adjusting it accordingly isn’t just a good idea; it’s the only solution possible for any problem that doesn’t conveniently lend itself to exhaustive exploration each time.
These are some good comments on bias, thanks “Refreshed.” You said what I have been thinking, but articulated it better than I could have :-)
Pot kettle black
Thank you sir or madam. Please stay in the game. Your observations are vital.
Wonder what other creative uses they will find for being able to monitor blood pressure from afar without one’s knowledge
See which customers in line are the most irate?
No need to do that – they’re probably all angry!
Perfectly make sense for monitoring blood pressure of someone who you don’t want to let them know, and for person who lost their limbs.
Next step, remote lie detection.
Except that lie detectors are bogus.
Until now…. And there is that existing IR camera setup that looks at blood perfusion around the eyes. Galvanometric lie detecting is bogus if used on its own.
Hmmm… Sounds like shades of Blade Runner.
Maybe not full lie detection but I wonder whether this would be a fun/weird addition to video dating. To gauge interest and reactions rather than lying– heart rate and blood pressure. And imagine doing a job interview with this in real-time.
The good thing about this method, if perfected, is that it allows for fast and frequent measurements in the context of other biometrics and this will help to even out the error in blood pressure measurement where results can be skewed by something as simple as posture or the timing and size of your last meal and defecation.
My blood pressure is always higher in the doctor’s office. As in having the same person with the same equipment measure it the waiting room instead of the examination room will give a reading 10 points lower.
Literally called “white coat hypertension”. Well documented.
I’m exactly the opposite. When the doctor checks my blood pressure, it is always normal. When I go about my daily life, it is always too high.
The difference is that when the doctor takes my blood pressure, I’ve usually just spent half an hour (or more) relaxing in the waiting room with something to read. My blood pressure drops to normal when I read.
The only way to tell if my blood pressure is really too high is to do a 24 hour test. The doctor puts a cuff on you with a datalogger. It checks your blood pressure during the course of the day. That shows that my blood pressure is too high most of the time.
The exception was the one time the (attractive) nurse who put the cuff on me for a 24 hour test managed to rub my arm and hand all over her front side. The doctor looked at the first readings from the datalogger and assumed it was the “white coat syndrome.” It wasn’t. It was the “OMG. Stop rubbing my hand on your protuberances” syndrome.
When I measure my BP, I get so nervous about the measuring itself that I need to repeat it four or five times and watch the numbers go down each time, basically caused by hypochondriasis. If the reading doesn’t go down, it starts to go up until I can calm myself.
That’s like my mother-in-law. When she doesn’t feel well, she checks her blood pressure. It’s usually a little high, so she gets nervous and drives it up. She then checks her blood pressure again, and it’s higher. Repeat with the pressure spiraling up until she calls my wife to take her to the doctor.
No mention at all about how these readings are affected by skin color? It’s well known that facial recognition doesn’t work well for dark skinned people, is this more of the same?
Facial recognition requires training – and the earlier systems were trained on predominantly white people. But yes, skin colour will affect this, as it affects photo oximetry (which is especially bad on reflective systems that watches use). But neither of these I hope will be used in a clinical setting, or to dactually diagnose anything, its just for the worried well as something to measure and be interested in.
Maybe the readings are not affected. Perhaps that’s why it’s not mentioned. Or maybe it is. You should probably contact the developer directly instead of pontificating on some random forum.
The paper states the subjects had a variety of skin tones.
Slowly getting closer to Tri-Corders and Dr. McCoy’s diagnostic bed. It would be nice to go to a doctor’s office and have all the vitals taken non-intrusively and quickly. (I want to take a Time Delorean into the future and bring back “Bones”. He would have solved Covid in 30 minutes. 😁)
Well another ability to add to a tricorder.
Interesting stuff. Perhaps not ideal for accurate one time assessment, but regular monitoring over time could be a good application at home.
As a stroke survivor living with hemiparesis, I ought to be monitoring more regularly but dealing with a chic is such as hassle. Especially since it needs to go on the unaffected arm. The affected side tags 10+ points lower.
And the act of fighting with a cut raises my BP, too. :)
I wonder how long it will before this technology is being abused by advertisers and implemented into CCTV everywhere, probably starting with places like airport scanners.
It’s a pretty terrifying prospect for the invasion of privacy that could potentially follow.
Imagine walking into a shop and being directed to a pharmacy for blood pressure medication.
IIRC, This is built off of the video motion magnification technique developed by MIT (again, IIRC. Even though a handful of companies are making claims its special proprietary algorithms, MIT makes a lot of their algorithms available free online. A bunch are on github). Steve Molde has a few videos featuring motion magnification and detecting a pulse via differences in skin color this type of video frame processing/computer vision.