[Gui Cavalcanti], whose name you might recognize from MegaBots, got on a call with a medical professional in San Francisco and talked about respirators. The question being, can we design and deploy an open source version in time to help people?
Unnerving reports from Italy show that when the virus hits the susceptible population groups the device that becomes the decider between life and death is a ventilator. Unfortunately they are in short supply.
The problem gets tricky when it comes to what kind of respirator is needed CPAP, BIPAP, or Hi-Flo oxygen NIV are all out. These systems aerosolize the virus making it almost guaranteed that anyone around them will get infected.
What we need is a Nasal cannula-based NIV. This system humidifies air, mixes it with oxygen and then pushes a constant stream of it into people’s lungs. If we can design a simple and working system we can give those plans to factories around the globe and get these things made. If the factories fail us, let’s also have a version people can make at home.
If you aren’t sure if a ventilator is something you can work on there are other problems. Can you make algorithms to determine if a person needs a ventilator. Can we recycle n95 masks? Can we make n95 masks at home? Workers also require a negative pressure tent for housing patients. This will be especially useful if we need to build treatment facilities in gyms or office spaces. Lastly if you’re a medical professional, can you train people how to help?
Let’s beat this thing. The ultimate medical hackathon begins.

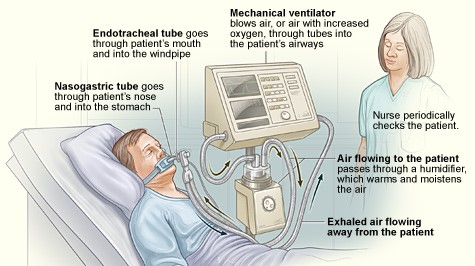












Percussive ventilation is very rudimentary. They use pressurized oxygen and simply have a regulator, a valve and a flow amplifier (e.g. venturi).
Why not 3D print the Army Emergency Respirator? It’s essentially a block of Lucite with channels cut into it attached to a mask – it has no moving parts. If somebody could find a diagram it would be easy to manufacture
Andrew: That solid-state design sounds fabulous; it would be great to see schematics & documentation about the Army respirator—please post ‘em if you got ‘em! Assuming it’s made by layering channeled slabs of Lucite together to build complete pathways, this tech isn’t being used to its full potential in fluid processing, though microfluidics people are receptive. Transparent polymer makes sense because obstructions can be seen.
https://www.reddit.com/r/AskMeddit/comments/flcrom/1965_army_emergency_respirator_is_a_ventilator/
What is the pressure differential in psi during lung expansion and exhalation. It seems that requirement is related to bodyweght. But a probelm used to be damaging jings by overpressure. C19 damages the lung.
This conversation is informative and full of excellent ideas. Has someone summarized and provided links to people acting on this topic? @dammitcoetzee , maybe? Does the hackaday platform support an FAQ?
A major joint hospital and university urgent challenge “to design a simple, low-cost, easy-to-manufacture and easy-to-maintain ventilator which could be deployed anywhere needed to save lives” by March 31 is underway. See “Code Life Ventilator Challenge”
https://www.mghfoundation.com/en/news/code-life-ventilator-challenge/
Discussion board for Ventilator Challenge at agorize, “discussion” tab, (requires registration with agorize)
https://www.agorize.com/en/challenges/code-life-challenge
looking for a mechanical /bio-med/ engineer with knowledge of pneumatic-=gases equipment. I have a design for a small portable ventilator that is simple and easy to make. I am a Respiratory Therapist and EMT Combat medic with 30 years experience. I have a design -with some help-could be fielded in less then a week. Someone interested in making a difference, contact me-bill2resist@gmail.com
Bill: Have you encountered the Army Emergency Respirator mentioned by Andrew recently? No need to reinvent the wheel if that one’s already got what’s needed.
Hello, I found this crouwdsourcing ressource : coronavirus tech handbook with a section dedicated to the ventilators.
I can really help with that but that could be usefull to someone here
https://coronavirustechhandbook.com/ventilators
Regards
Hi,
I am a critical care/flight nurse. The problem with some “emergency” ventilators is that they are unable to deliver PEEP (peak end expiratory pressure). This is what the sick patients need; simply blowing air in and out does not work. PEEP for the really sick patients needs to be about 20 mm H20.
The most low-tech design would utilize a bag-valve (Bag-valve-mask or BVM) system, which is what is used before the ventilator is attached. A person squeezes the bag at the desired rate. A PEEP valve can be added to this system easily.
All that is needed is a strap to squeeze the bag at the desired rate (and the correct tidal volume). Mount it all inside some type of box…..
This is pretty close to what you are describing.
https://web.mit.edu/2.75/projects/DMD_2010_Al_Husseini.pdf
Hi Mike,
This initiative would definitely appreciate your expertise & experience! https://opensourceventilator.org
Late to the string, 30 years manufacturing and fabrication including medical yada.. Being older and fatter than most of you, CPAP and similar systems are now dirt common and do several pieces of this puzzle especially pressure, masks and hoses. I throw that stuff away regularly. Apologize if this has already been exhausted. Welding 02 and some way to control exhaust for spreading infection. Not to happy to entubate myself but hey, in a pinch.
Founder / CEO, FLEDGE Innovation Labs
Medical Devices Incubator
40+ years developing / commercialising medical devices
=====
Steve Redmond (March 15, 2020 at 3:39 pm) is 100% correct …
This is not a DIY project.
We cannot solve this problem using garden hoses and vacuum-cleaners, or by passing exhaled air though buckets of boiling water.
>>> WE NEED TO USE WHAT IS ALREADY OUT THERE <<>> WE DO NOT HAVE TIME TO DEVELOP A NEW PRODUCT <<<
We need to find ways to scale up production of existing products, and to re-purpose existing products to meet the current need, based on available resources of equipment, oxygen, electricity and people.
Regulatory IS an issue, but we can't let that hold us back – there are ways of fast-tracking solutions to meet medical device standards, but we cannot cobble solutions together in our garage – it's just not scaleable.
No matter what product is used, we also need the infrastructure to support it. There's no point making 30,000 ventilators unless we have enough people trained to use them, particularly when we see survival rates of 3% in China for ventilated/intubated patients.
We need to focus our efforts on slowing the rate of admissions to ICUs, and supporting people in a pre-clinical environment.
What we need is a SIMPLE solution that supports patients BEFORE they develop Acute Respiratory Distress, even its only for long enough to allow the health-care system to build capacity.
Bench Tests of Simple, Handy Ventilators for Pandemics: Performance, Autonomy, and Ergonomy,
http://rc.rcjournal.com/content/56/6/751
‘Pandemic ventilator’ could offer solution in potential ‘worst case’ coronavirus scenario”
https://www.cbc.ca/news/canada/london/pandemic-ventilator-coronvirus-hospitals-1.5493830
“ASPR supported the development of a portable ventilator capable of providing mechanical respiratory support for critical care of newborn babies, adults and elderly patients. The Philips ventilator was cleared by FDA earlier this year for use in institutional, home, and field settings by minimally trained operators and is now stockpiled in the Strategic National Stockpile for immediate distribution when needed.”
https://www.phe.gov/ASPRBlog/pages/BlogArticlePage.aspx?PostID=367
Ventilator capability and capacity requirements, in old issues review paper, “Guidelines for Acquisition of Ventilators to Meet Demands for Pandemic Flu and Mass Casualty Incidents,”
https://www.aarc.org/wp-content/uploads/2017/03/Issue-Paper-Acquisition-ventilators_pandemic.pdf
BARDA Funds Development of Next-Generation Portable Ventilators
https://www.infectioncontroltoday.com/epidemics-pandemics/barda-funds-development-next-generation-portable-ventilators
But I have not found the results of this project announced in 2010. (??)
How about human assisted breathing device
two masks hot water bottles coupled through scissor type mechanism a loved one can help the patient breath no peep or volume or pressure issues
if you have power then think about heating the air
next step mixing in oxygen
Thanks OZ B ..
Your HWB solution is very inventive, but remember that these patient have compromised respiratory function.
If a patient is so sick they cannot breathe on their own, their lungs are already facing and very likely they have pulmonary sepsis /pneumonia, kidney failure, liver failure and need sedation / antibiotics etc.
What will be patient do when the loved one has to go to the bathroom ?
How will this scale to 30,000 people ?
‘HOw will you know whether the patients is improving or getting worse ?
This is very complex – a lot more than moving air from a to b.
Thebest thing to do is let ventilators manufacturers make ventilators, and their experts, which have decades fo=of experience with this – come up with other solutions.
We can support them by propping up the supply chain, avoiding panick-buying, reducing the load on suppliers, staying at home and making sure we dont compound things by spreading the virus.
That appears to be a ventilator helmet, the stop gap device needed assp!
Ventilator Classification
https://slideplayer.com/slide/7474105/
I’m looking to reduce the spread by figuring out the proper substitute materials to make masks in this current shortage. I understand the melt-blown fabric used for n95s is in short supply currently and can’t get here soon enough but there are studies comparing other fabrics to surgical masks and n95 ones. I’m looking specifically to figure out a combination of woven and non woven fabrics that can get our HCPs closet to a surgical mask and well above a bandana when combined with a face shield for effective PPE. Also hoping these can be used by the public to reduce spread. Anyone else working on this angle or able to offer up additional info?
My sources so far:
https://www.ncbi.nlm.nih.gov/pubmed/27531371
https://www.npr.org/sections/goatsandsoda/2020/03/16/814929294/covid-19-has-caused-a-shortage-of-face-masks-but-theyre-surprisingly-hard-to-mak
https://www.providence.org/lp/100m-masks?fbclid=IwAR0b8Edl5F2gi7LVI2QtLJyEAnpG9M5KBJiYlPZGE9eYePFj3Do3xvlOyDM
What about vaccum cleaner bags, there is a study/comparison of different materials for mask use and the vacum cleaner bags was the best of compared materials.
https://www.researchgate.net/publication/258525804_Testing_the_Efficacy_of_Homemade_Masks_Would_They_Protect_in_an_Influenza_Pandemic
I would like to contribute to this project. Aside from leaving comments, is there a place for drawings, diagrams, algorithms, etc?
Thanks
Mac McClanahan
Look at the pictures at the bottom of the (sorry all in german) Link…obviously, for hyperbaric oxygen therapy you’d only need a sealed hood, a mechanical air pump and yes, Oxygen. One could bring together an emergency CPR mask (for the valves) with any kind of plastic bag by using a shrink wrap, cover patients head with it, seal it around the neck, pump it up and administer the oxygen = “bubble hood”….no?
https://www.bergsteigen.com/news/expeditionen/tar-helm-zur-ueberdruckbehandlung/
Some random thoughts:
I think that air is easy to supply using consumer equipment. Plenty of vacuum cleaners provide about the right pressure and enough flow for an entire ward.
The challenge is the demand valve (servo sleeve valve). it needs to take a large volume flow at low pressure so it has to be about two inch bore, but it doesn’t need to be high pressure. Maybe irrigation systems are where to look. The other challenge is the mask which must seal against enough pressure to get the lungs inflated. I have no idea where to get this.
As to oxygen, The simplest way is to manually bleed this into the air flow from a bottle at a rate informed by the patient’s blood oxygen monitor.
The logistics of providing oxygen in bottles may be a limiting factor. Far better to consider domestic oxygen concentrators but if commercial models can deliver at the required rate will require further investigation.
uk open sourced design https://www.gov.uk/government/publications/specification-for-ventilators-to-be-used-in-uk-hospitals-during-the-coronavirus-covid-19-outbreak
Would an off-the-shelf server UPS do for battery backup?
Miscellaneous Part 6
“c. Ideally instructions for use should be built into the labelling of the
ventilator, e.g. with ‘connect this to wall’ etc.
d. Must include clear labelling of all critical functions and controls using
standard terms, pictograms and colours that will be readily recognised
by UK healthcare staff. ”
That’s probably pretty damn important because on 72 hours no sleep med staff are gonna be uncomfortably close to …
https://www.youtube.com/watch?v=hmUVo0xVAqE
So what is the liabilty to the hospital or person producing a 3D valve if fail occurs?
I would actually like to start making a ventilator as soon as I can.
There is a lot of technical details I am not in a position to understand quickly.
I learn best doing something and working with what I have around me.
I hand drew up a design I think I could make in my shed (see link below)
First I need to know if I have understood the concept correctly.
Then I need to fine tune the details.
I want to keep the main elements modular so as and when improvements are available they can be swapped out.
1) Variable air pump
2) Filters
3) Air temperature control
4) valves + oxygen mixing
5) Air pressure regulation
6) sensors
7) electronic controls
The simplest design I could think of that I could make was to use two bellows on a rocking frame.
The sketch shows how I imagine the bellows would hang and be driven using a stepper motor and belt drive.
I have built several off the shelf 3D printers using Arduino based electronics so it looks feasible.
I think keeping all the valves in a central box with the sensors will focus the complexity away from
other areas of the build. I need help with this and electronics.
It also occurs to me that this design (assuming it has merit) will be flexible in using the widest
available resources like: off the shelf components, wood, metal, plastic, glass, plumbing, motors, electronics, etc.
If someone can take the idea to the next level in design and specification so I could build one;
Or direct me to a viable alternative design I would be very grateful.
Thank you :-)
Sketch is here … https://fixgrowmake4health.blogspot.com/2020/03/coronavirus-covid-19-open-source.html
For the algorithm that determines whether a patient requires a ventilator, I have completed one such algorithm. The prediction component is aproxximately 88% accurate as determined by RMSE. Heres a link to my Github Repo. Any and all ideas for improvement would be welcome.
https://github.com/bugbamboo/m3-or-Coronavirus-help
Just spoke with a friend who is an ER doc in NJ who recently published this oped – https://www.nydailynews.com/opinion/ny-oped-what-a-war-footing-really-means-20200315-rdraci7atreczmmf4mtoiru76i-story.html
He said they could really use the following (and believe it could be made using 3D printing):
http://www.strac.org/files/Manuals%20&%20Guides/Vortran%20Automatic%20Resuscitator%20User%20Guide%202005,%20Apr%2014.pdf
They need this because it is small, portable and doesn’t require electronics or electricity. It runs using air pressure. And although they’re designed to be single use, they could be cleaned and sterilized for reuse if necessary.
If you can help, please contact Dr. Kamal Kalsi at maplelotus@gmail.com
For mass ventilator to supply multiple patientes at once, could you adapt a central vacuum system drawing fresh air and using exhaust piping with individual tubes feeding multiple beds along the line. Regulators could be installed at each line to control air flow to each patient. The intake area could be enriched with constant injection of O2 / humidity. Quick and easy set up for field hospitals etc. Just a thought I had while cleaning my central vacuum system. It draws and pushes a lot of air.
Greetings Gents,
Is this xploded view drawing from Ventec of any help?
https://www.venteclife.com/
https://techcrunch.com/2020/03/20/gm-and-ventec-life-systems-partner-to-ramp-up-production-of-ventilators/
We need an image of a ventilalor
Ozone generators can be used to sterilize masks and respirators. N95 masks should be good for many reuses after sterilization. To sterilize a few masks at a time buy a CPAC cleaner like one of these: https://www.amazon.com/sk=cpap+cleaner+and+sanitizer&i=hpc&crid=3FSL30C37Q571&sprefix=CPAC+cl%2Chpc%2C190&ref=nb_sb_ss_sc_1_7 I suggest buying the small cheap battery powered units that come with a small bag. You don’t need a hose. You can place the generator and the masks in the bag.
To sterilize many masks at a time buy a big ozone generator that can fill a whole room with ozone. https://www.amazon.com/s?k=Ozone+Generator&ref=nb_sb_noss However, ozone will severely damage lungs so be sure the room is sealed and wait the recommended time (at least two hours) before reentering the room.
Ozone if efficient can also be used to sterilize a boot full of groceries on the way from the shop to the home, hopefully without damaging the goods.
UX Designer and coder here.
Not sure if I can help with the construction, but once there is one that works I am happy to design the instructions, manuals and websites so that everyone understands it. Hope that helps.
You may be able to hack an electronic oxygen conserver regulator into a ventilator. Oxygen conservers are regulators that are used with oxygen tanks to supply medical oxygen. They make the oxygen tank last longer by sensing when you are taking a breath and delivering a pulse of oxygen at that time. Some conservers are completely mechanical and would not be of use. However, some conservers are electronic. An electronic conserver has an electrically controlled air valve. You could connect the electrically controlled air valve to a simple 555 timer circuit and control the duty cycles with potentiometers. It would probably be a good idea to insert an airbag between the valve and patient to buffer pressure spikes. You need to be sure that the changing pressure of the tank won’t change the delivered volume of oxygen. The conserver probably already does that with a built in upstream regulator. Here is a link to an electronic oxygen conserver.
https://www.drivemedical.com/us/en/products/respiratory/oxygen-therapy-%26-accessories/oxygen-therapy/smartdose-mini-auto-adjusting-oxygen-conserver/p/300-1
We need to increase production of helmet ventilation systems. Basically a plastic sealed hood with an oxygen port and exhale valve attracted to a filter. They have been shown to reduce the need of intubation for people with ARDS. They do not require ventilators just high flow oxygen. Cpap ,bipap HFNC, all have been shown to increase spread of the virus.
Yes Sevenhuis – you are spot on.
These helmets provide oxygenation support and control aerosols – which otheriwise infect health-care workers,
turning them into patients – which threatens the stability of the healthcare system.
But let’s not call them ventilators – they’re non-invasive and used for people who still breathe spontaneously.
They provide oxygenation – not ventilation in the sense of assisting someone unable to breathe on their own.
>> WE DO NOT NEED VENTILATORS <<<
We need oxygenation support – not ventilators.
Your right Gary they are non invasive and only help with oxygenation and not ventilation but the study out of Chicago in 2016 showed significant reduction in intubation rates and all cause mortality. This is the approach we should be addressing in this hack not ventilators.
Yes Sevenhuis – you are absolutely right.
This thread is addressing the wrong question – we should be asking :-
Q : What can we do to to maintain oxygenation for people presenting to hospital with Acute Respiratory Insufficiency resulting from a COVID-19 infection ?
NOT …
Can we make a complex device like a ventilator using parts from the hardware store, to solve a problem we don’t understand, and train people on how to build it, deploy it and maintain it, and monitor patients on it, and deploy it at scale, globally, in a highly regulated environment in less than a month ?
I am working with two seattle doctors (ED and ICU) and a growing team of engineers to build an open source CPAP helmet. I live in northern italy so I’m hoping to get a real model to the US for evaluation. The helmet isn’t super complicated, but of course mass production is. Right now a company called Sea Long in Texas makes a similar device that can be modified for CPAP therapy. My biggest concern is FDA approval, but maybe I’m getting ahead of myself.
Hey all! I have a ventilator system concept that I think solves several of the major challenges presented (especially cost and material availability), but will need a lot of prototyping to determine if it’s viable. You can view it here: https://github.com/jwilson8767/covid-19-ventilator-concept
I have no additional intention to participate in this hackathon (IS this even a hackathon?), but please ask questions and provide feedback and I will incorporate into this concept.
Could scuba gear not help?
Peter: Thanks for mentioning SCUBA, which pushes air into the lungs when the person initiates the breathing cycle. It would be great if a respiratory therapist who dives could contribute to this discussion, because they’d know whether ventilator patients are able to provide enough initial aspiration. SCUBA air regulators adjust air pressure to compensate so that shouldn’t be a problem.
I think Tyvek house wrap is good enough for making masks to protect the healthcare workers from the Coronavirus. I’m not sure how many layers we would need to use in making them?
Maybe, we could gather the supplies from Lowes, Home Depot, etc. and start hand producing them.
So you are telling me you don’t need actual ventilators “CPAP, BIPAP, or Hi-Flo oxygen NIV are all out.”
Sounds like this article is BS.
Our current CPAP, bipap systems in the USA have shown to spread the virus in hospitals. Current recommendation is to use nonrebreather face mask, once o2 drops on this therapy to intubate. No cpap or bipap. This systems allows positive pressure oxygenation without the risk of virus spread. Italy is currently using this system to help with the ventilator problem. The study was small I agree but given the choices I believe it is a better option than we currently have.
Hello Sevenhuis,
Yes – as usual – you are 100% right.
BUT – studies have also shown that a P2/N95 mask worn by a patient on high-flow NIV produces aerosols at about the same rate as a non-insufflated patient without a mask.
https://vapotherm.com/covid-19-resource-center/
IMHO we need to avoid intubation wherever possible – and provide pre-transitional support to maintain O2 levels.
We need more of these …
https://www.dailymail.co.uk/news/article-8134247/Bubble-helmets-used-Italian-doctors-boost-survival-rates.html
We also need a way to monitor SpO2 simply and cheaply – so patients can be more effectively triaged when equipment is in short supply – thats a project we’re working on at Fledge Innovation Labs.
Hi Jesse,
I’m not sure what your background is, or whether you’ve ever been involved in patient care, or whether you’ve ever developed a complex medical device and taken it to production and seen it save lives – I know I have.
I’m not sure what you mean by saying “CPAP, BIPAP, or Hi-Flo oxygen NIV are all out.”
If you’re saying these cannot help, then you’ve been misinformed.
Each has it’s pros and cons, and in many circumstances they would be helpful, if not ideal.
The man issue is that these machines produce aerosolised virus which infects healthcare workers. This turns carers into patients, and the healthcare system unravels leading to INCREASED fatalities.
Look at the original challenge …
“What we need is a Nasal cannula-based NIV”.
NIV – NON INVASIVE – ie, not a ventilator.
Perhaps I should have been clearer when I said we dont need ventilators … of course we DO need ventilators.
What I should have said is that this effort should not be focussed on making a DIY ventilator, there are other much more effective ways to address this problem and get better outcomes.
Check my other posts.
Could something be designed to take the CPAP exhaust with suction into a HEPA filter or series of filters? Would this protect nearby health care workers?
Yes – that’s a good suggestion, one that’s been proposed previously.
One solution is for patients undergoing NIV HFNC therapy to wear a PC2/N95 mask – research indicates that reduces aerosols to the level of a spontaneously breathing COVID patient with no therapy.
That’s assuming there are enough masks of course.
We’d do much better by changing people’s people’s behaviour to stop wearing masks unnecessarily, and to stop hoarding masks and donate UN-used ones to hospitals for use by healthcare workers – who are running short.
I was in surgery today and they are SERIOUSLY short of masks – to the extent that some areas have no masks at all.
We need to stop trying to design ventilators – its a waste of time.
I would be MUCH more effective to help existing manufacturers of masks, canals, oxygen tanks, ventilators etc re-establish their supply chains. Contact your nearest manufacturer and find out what they need to ramp up production – whether its parts, materials or labour.
I thought this project might be a little ambitious considering the time and materials required. I think your suggestion is a good one. I’m going to put my energies somewhere else. I will monitor this page though and if you do have something you want to bounce off me please feel free to reach out.
Mac
I’m a 3D artists who specializes in medical renders and animation… if you have concept art or idea needing fleshed for funding or proof of concept regarding visuals, I’m more than happy too help… it’s the only way I can really ” in lockdown atm”
cheers
@IdoineTutorials – twitter
Problem is all this DIY respirator groups are popping up trying to reinvent the wheel. Why don’t just post the inner workings of an actual machine so we can figure how to simplify it or DIY its parts? It will be a lot faster than trying to invent something we never worked with neither know the specifications and what works and what doesn’t work.
Could used n95 masks be autoclaved and made sanitary again?
Negative pressure ventilation is easier on the lungs.
It is low tech And could even be built in any home shop with few basic tools. It’s the old iron lung technology tested over a hundred years and proven during the mid century polio epidemic. There was a company in Colorado called Porta Lung that made a modern version but I don’t know if they are still around. If you want to build an iron lung here are plans from 1952 http://blog.modernmechanix.com/diy-iron-lung/
It could easily be simplified with modern controls and motor.
Sorry if this comes up twice don’t see my reply.
The last epidemic that needed massive amounts of lung assist was polio in the 1950a. They used iron lungs to keep people alive. There were entire wards of them and they were easy enough to use and low tech enough that many people had them in their homes. They were even home built http://blog.modernmechanix.com/diy-iron-lung/
These could be knocked out in every shop in the country and could be fabricated out of wood plastic sewer pipe, propane tanks, spiral duct or anything you could get your hands on and had hand tools to work on it.
The tech is way past patent. Could be easily updated to simple motors and controls you could even use a shop vac in a pinch.
There was a company in Colorado that made an updated version that was portable with a separate vac unit until a few years ago. Porta Lung. They still have a web site but I think they just handle medical supplies now.
The kicker is that iron lungs use negative pressure ventilation (npv) it doesn’t have the problems of ventilator induced lung injury (vili) that positive pressure ventilators (ppv) do. Oxygen can be administered to the patient through a mask at ambient pressure just like always with no pressure problems. As near as I can tell they quit using iron lungs in medical settings because they were cumbersome and new ppv left the whole patient open to treatments without going through ports.
The last of the iron lungs went away in this century after being used for 50 to 60 years by their owners. Some of the old ones even had hand pumps in case of power outages. Looks like what’s old is new again to me.
Heres my design so far https://www.thingiverse.com/thing:4235537
Hi there,
Just wanted to pitch an idea which might be completely useless/dumb or quite simple (product designer not an engineer or somewhat close to medically educated).
I read some of the posts and saw a few about welding oxygen. The idea is as follows:
– instead of supplying oxygen through the mouth/windpipe inject oxygen directly into the (preferably lowest) part of on of the two lungs. This will eliminate the need for a ventilator/pump by using the windpipe/mouth/nose as an exit for the gases (CO2) an abundant 02 that would normally be exhaled.
– add some sort of waterpipe system in between the welding gas tank and patient to humidify the air pumped in
– a reverse pressure valve that closes instead of opens at a certain pressure.
– smaller risk of blowing out a lung due to the gasses always having an escape route???
– lungs close to fully expanded making them more efficient???? Do patients need the breathing motion? If so add valve that closes the flow from the tank to let the patient exhale themselves
here is your opensource ventilator: https://www.oxygen.protofy.xyz/
seat spain similar prototype: https://twitter.com/tierraymadera/status/1241662339528773632
They have just achieve to certify it. It is open source, with 2 designs, one for makers and another for mass line production.
Hello
I did my training in medicine in India in late 1980s and as a house officer we used to do different things for ventilator needs as there were only 2 ventilators in our entire university hospital. Many times we junior house officers ended up ventilating manually in turns a patient whole night with just an ambu bag.
The design I am suggesting is a large piston cylinder like equipment with 6 or 10 plastic ambu bags on one end of the cylinder and a piston pushing it down in regular intervals (about 15/minute) compressing all ambu bags together and each ambu bag could be connected to each patient through tubing. Each ambu bag could get oxygen separately, the flow could be adjusted individually. This equipment could be operated manually by a person (with the help of a liver) or by electric powered, and could be connected to 6 or 10 patients at a time, depending on the number of ambu bags it has.
Basically what I am suggesting is a cylinder- piston equipment with multiple ambu bags , which are all compressed together with a piston. The ambu bag can be designed like the plastic vacuum creating bags used in small surgical drainage systems used for seroma drainage, which would allow compression by a piston.
What about a Biphasic Cuirass Ventilator or BCV. It is completely external and can be used outside of a hospital, works with supplemental oxygen systems and does not require a highly trained medical technician to operate. The BCV evolved from the iron lung used to treat Polio victims in the twentieth century but it is now chest sized and uses a portable pump to work. It is an FDA approved medical device. One key capability of the device is an active exhale assistance (think assisted cough) that can help patients clear their lungs. It doesn’t use a mask so existing supplemental oxygen systems can work with it.
Absolutely. It is a bit higher tech in its normal vacuum driven system and needs a more complex deal to be able to have universal fit.
Would a Both respirator iron lung work for covid19? These things are dead simple and we’re built out of plywood in the 1930’s for polio victims. https://en.wikipedia.org/wiki/Both_respirator
Exactly. There are links to an article from a 1950s magazine with plans to build your own plywood iron lung. Guess it would be a plywood lung. Sorry about that. Just needed to lighten up for a moment. Porta Lung in Colorado was making a modern version of the iron lung. I contacted them and was told they still keep their certification up to date to produce theirs.
This is worth a look..
https://www.youtube.com/watch?v=oS6GA83nbds
Sorry, since i am german i almost don’t dare to share following input here, but i think its worth a glance anyways: What about sealing off whole rooms and transform them into positive pressure chambers, then flooding them with additional oxygen …you know… would spare masks and pipes and stuff…you could treat a max of people at the same time as long as they are able to breath by themselves at some level….
No?
Good luck to all of us and y’all stay safe! Best. S.H.
I was thinking about the same thing only with negative pessure and each patient with a sealed mask and hose to exterior ambient. Then it seemed to get more complicated and I went back to single source negative pressure.
From what is known of this sort of technique it doesn’t sound like a very promising treatment in this case…
https://en.wikipedia.org/wiki/Hyperbaric_medicine
In Italy they succeeded to make a working ventilator from scuba gear and 3D printed parts.
https://dgiluz.wordpress.com/2020/03/23/its-working/
Yes Susanne, that has been used in some cases.
BUT – the downside is that is does not control virus-laden aerosols exhaled by patients.
Health workers get infected, turning them into patients, which means there are less people available to care for the sick, leading to INCREASED fatalities.
An oxygen-enriched room becomes unstable if the O2 level gets too high – as happened in Apollo 1.
Also, there is bound to be an oxygen shortage, so O2 needs to be carefully used and contained, which is extremely difficult to do in rooms not designed for the purpose – and in a short timeframe.
Use a shop vac. The inlet side passes thru a filter and the exits thru the exhaust side. Hook the hose to the exhaust side for the ventilator hood for the patient. Use a water meter gauge to measure exit pressure. The inet side could be regulated to drop the pressure if needed. If humidity needs to be added. Put water in the shop vac. Use some kind of heater to make humidity as the air passes thru the shop vac.
Use the shop vac to create negative pressure ventilation and the rest is done as usual with gas delivery system that is already at every hospital bed in the country.
consider using a BVM as the main part and just build a squeeze mechanism as the BVM is already an approved medical device greatly reduces and alleviates a lot of medical concerns. Just need a way to control depth of squeeze and frequency.
Proposal of an opensource project respirator for 40 Euros – from a 3D printer from Poland. This project is open source proposal for epidemic situation in the world. https://www.europeanscientist.com/en/public-health/an-open-source-respirator-for-40-euros-from-a-3d-printer/ or https://www.ventilaid.org . Perhaps it’s help to make other better project 3D or help in this shape country.
https://www.dailymail.co.uk/news/article-8147119/Family-run-engineering-company-develop-ventilator-just-THREE-days-treat-coronavirus-patients.html
This project is looking very promising…. such a simple design ! https://oxvent.org/
Yes – I posted this earlier.
Also this.
https://patentimages.storage.googleapis.com/22/ce/16/6fb96f2bc99ff4/US4620538.pdf
It’s a demo that an Ambu bag can be operated using compressed air.
The issue is that Ambu bags are normally operated by a skilled HCW who adjusts depth and frequency to suit individual patients – the HCW provides the feedback loop.
ALSO – it depends on having a compressed air supply – which sort of defeats the purpose when you think about it, when the purpose of manually operating the bag is to provide compressed air.
If you have compressed air, you dont need an Ambu bag.
What you do need is a source of oxygen enrichment and a means to control it automatically, based on a patients condition.
Remember the Ambu bag is for patients unable to breathe spontaneously – and there is a looming need for that.
But what we need to focus on is supporting patients so they dont get that sick – by providing O2 enrichment therapy to slow the onset and severity of respiratory distress.
I’m looking for quick diy home hacks in case all public resources are not available.
What if I used electolosis to generate concentrated O2, and used my air matress pump to force the O2 through a snorkeling mask?
https://www.nxp.com/docs/en/application-note/DRM127.pdf
A great reference design for an open source ventilator from NXP.