Hackaday, we have a problem. There are a lot of people on this earth and not a lot of health care workers. Let’s use our skills to help alleviate this problem. What can we do to give medical professionals a wider reach, to bridge the distances between hospital and patient, and make it easier for bystanders to administer lifesaving care.
Scope of the Problem
We’d wager that your most recent and vivid remembrance of a health care worker shortage is the Ebola outbreak in West Africa. The shortage of trained professionals and supplies certainly compounded the situation in the countries worst hit. But it didn’t create the problem. Check out this list of doctors per 1,000 people (sorted lowest-to-highest with 2010 numbers). The three countries hit hardest by the outbreak — Guinea, Liberia, and Sierra Leone — register a whopping 0.0 doctors for every 1000 people. Yeah, that’s years before the outbreak.
Keep scrolling down and you’ll see that this isn’t limited to one geographic location. All over the world there are low numbers, with India and Iraq both at 0.6, and interestingly Cuba and Qatar topping the list at 6.7 and 7.7 respectively.
This isn’t a statistics post so let’s pivot. The point is made that we’re a large world population. What kind of engineering solutions can we wield to help provide everyone with the care they need? Leave your comments below but also considered entering the Hackaday Prize with them. Write down your idea as a Hackaday.io project and tag it 2015 Hackaday Prize.
Proof That We Can Do This
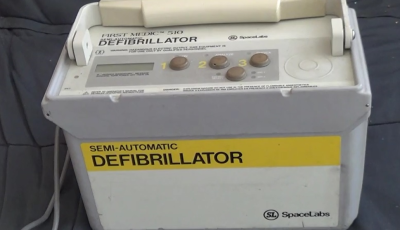 It’s safe to say we’ve all seen engineering solve part of this problem already. Over the last decade, Automatic External Defibrillators have become ubiquitous. The life-saving hardware is designed to be used by non-doctors to save someone whose heart rhythms have become irregular. [Chris Nefcy] helped develop AEDs and one ended up saving his life. If that’s not proof that we can change the world with our builds we don’t know what is.
It’s safe to say we’ve all seen engineering solve part of this problem already. Over the last decade, Automatic External Defibrillators have become ubiquitous. The life-saving hardware is designed to be used by non-doctors to save someone whose heart rhythms have become irregular. [Chris Nefcy] helped develop AEDs and one ended up saving his life. If that’s not proof that we can change the world with our builds we don’t know what is.
Pull on that thinking cap and jump into this conversation. What can we build? What problems need to be solved right now? Where should each of us be looking to make a difference in the availability of health care in the absence of the trained professionals?















Replace patients with robots. ;-)
Okay, so much of the other feel good topics in this series have to do with chipping away at the edges of the resource scarcity problem and now you add the means to make that resource scarcity even more severe.
The first world has illustrated the problem caused by readily available sophisticated medical care. A proliferation of self inflicted diseases (heart disease, diabetes, etc.) that are largely produced by the poor choices of the people who then suffer from these diseases. And instead of them being forced to change the basic behaviors that caused the disease we provide them readily available (but extremely expensive to society) medical care to treat the symptoms of their poor behavior.
This does not seem t0 be a good model to extend to seven billion people. Especially when on considers that the wealthiest countries in the world are finding it unsustainable.
It is a sad, but necessary fact of life that illness is a good thing. It helps control a population that refuses to control itself. Further, the probability of avoiding such illnesses that ‘medical treatment’ require is largely in the control of the individual if they simply follow some basics. Proper nutrition (something that is a much better use of scarce resources) and basic minimum levels of activity/exercise.
“It is a sad, but necessary fact of life that illness is a good thing. It helps control a population that refuses to control itself. ”
In two sentences you identify yourself as a sociopath. Congratulations.
“A proliferation of self inflicted diseases (heart disease, diabetes, etc.) that are largely produced by the poor choices of the people who then suffer from these diseases.”
A logical fallacy, the fact that some people with access to high levels of medical care make bad choices does not indicate that all people who access to modest levels of medical care will make bad choices.
But I agree that proper nutrition is a great use of scarce resources.
A knee-jerk reaction. You don’t have to be a sociopath to acknowledge that modern medicine defeats natural selection. That if medicine saves the life of someone who would otherwise die due to a genetic disorder, then that person goes on to reproduce and pass on that disorder, it increases resource use and dependence on medicine. Or that some poor choices are made due to lack of intellect or tendency to addictive behavior, both of which have some genetic basis.
That’s just the facts, and acknowledging it only makes one a realist. I do, yet I don’t like it. And I certainly don’t wish suffering or death upon anyone, nor would I ever want to be placed in a position where I would have to choose one life over another. If I did, THAT is what makes a sociopath.
+1. I agree completely.
It isn’t simply natural selection that is defeated. Without death matching at least the birth rate the population of any organiism will rapidly grow to consume all available resources which leads to the extinction of said population.
So ultimately which is better the death of some or the death of all. This is a simple either-or situation, at least if your not willing to take/allow dictatorial powers and start sterilizing your population. Because that is the only thing that will prevent the consumption of all available resources.
Your being ridiculous, we spend enormous quantities of money to postpone the inevitable. People die, and absolutely nothing will change that. If we slow the rate that they die (the absolute best we could do) we have the problem that they don’t slow the rate at which they reproduce. Something a planet with 7 billion people on it can’t really afford to do.
And we aren’t talking ‘some people’, nor is it a logical fallacy. Of the top five diseases in the first world, three are direct results of people poor choices. Yet we spend the vast majority of our health care resources to treat the symptoms of those diseases to allow those people to continue making their poor choices.
Ask a load of electronic and mechanical tinkerers to find a solution to some enormously intractable socio/politico/economic problem? Then spend millions putting ONE of these tinkerers in space because they used a teensy to blink a LED when it hears someone sneeze?
Meanwhile the poor buggers in the aforementioned stricken regions still keel over from malaria anyway.
10/10 for optimism though, HAD. :)
It has to do with risk/reward.
Hackaday has half a mil available. If they donate to malaria control, it will be less than a drop in the bucket, and go unnoticed among the many problems they could choose to address such as eBola, poor education, poor nutrition, war, and so on.
They could also buy a lottery ticket (the HAD prize), on the off-chance that someone comes up with a solution. It’s a cognitive bias, I know, but the sense of “doing something” by this method is more palpable and real than just adding money to the Bill and Melinda Gates foundation.
It also gets people engaged, which is a big problem in modern society. People feel disempowered and helpless with these issues – the problems are too big, there’s nothing any individual can actually *do* to help.
The HAD prize addresses this. Public engagement is important.
If you want to put this on a more firm foundation, consider the risk/reward equation in terms of financial investment. You don’t put all your money in secure, low-risk investments because a mix of low- and high-risks is more effective in achieving the goal.
This is just the other end of that analysis. A risky, “probably won’t work” investment, one that gets a lot of eyes on the problem and engages a lot of smart people into thinking about the issues, but it might pay off big-time and be more effective dollar-for-dollar than the safe investments.
I’ve got no problem with it. Your opinions may vary.
In technical terms, this is a solved problem. The answer is cell phones and some combination of expert systems and trained paramedics. The info is available in books like “Where there is no Doctor” “The barefoot doctors manual” and “The handbook of rural health” from the US GPO and various midwifery handbooks. These books are designed to train and be used by paramedical health workers who can handle 80% of health care and refer the rest to real doctors. Cell phone conferences with a doctor can handle half of what’s left and evacuation is the last resort. The problem is to get someone to pay for these unsexy but effective measures. The biggest health problems in the 3rd world are about malnutrition and bad water. Again these are economic not technical problems. Getting vaccines and drugs out to the hinterlands is a good measure but social resistance is a problem that can best be solved by having local health workers in the area who earn the people’s trust. Things like a low power simple to use ultrasound machine for imaging broken bones or a solar powered medication/vaccine fridge would be helpful but the biggest gains come from low end interventions like water filters and mosquito nets that are tailored to local problems and the best way to plan programs that work and get people to use them is to have trusted healthcare workers on the ground in the community. Equiping those workers with cellphones that can do common diagnostic tests will, again make them more effective, but a thermometer, BP cuff scale and tape measure will get you most of the way there if you know how to use them and what to look for. An expert system can tell you what to look for, but at a cost of time and treasure. The more you spend on training your workers the less you spend on IT, same as always. So, yes let’s see some Ideas, but the real root of the problem is how do we get basic infrastucture out to people who need it?
Three components remain that are required to make telemedicine applicable in the area with the most potential; specialisation.
The first is acceptance. Brian is totally correct in saying that local health workers are key to delivering care and changing attitudes. But they are also key to delivering specialised telemedecine. They need to be integrated, they need to be trained and they need access to the right loactions and people. They need the languages to talk to those people.
The technology, then, needs to be able to make the telephysician an acceptable part of the conversation – translation, interaction, both verbal and non-verbal cues. Talking to a doctor who doesn’t understand your language is terrifying enough in person. Trying to understand what they are meaning (not just saying) goes beyond the competence of the translator
The second hurdle is the examination. We have had telephones for a long time now but there’s a reason the GP doesn’t get you to put the phone on your chest to diagnose pneumonia (or at least they shouldn’t).
Accurately relaying this information has been achieved by training teleworkers on site to perform elements of the examination. This is imminently suitable for things summarisable as pure and repeatable numbers – blood pressure (stethescope, and sphygomomanometer or in a crisis a balloon, air pressure meter and valve, tubing and a sock), pulse and breathing rate (watch), Oxygen saturations (An oxygen sats meter. Saying “they’re pink” is not enough, thanks to carbon monoxide), weight, height and the like.
However the qualitative ones; the sound heard through the stethescope (an at which points that sound was, compared to others), the degree of respiratory effort (to a finer scale than none, normal, increased, extreme), the area, depth and pressure at which the patient screams from their abdominal pain.
Some of these have been tried, with varying sucess. If you don’t have a hearing aid, the electronically amplified stethescopes seem grossly incapable of representing heart sounds and murmurs accurately enough for a paediatric cardiologist; Video succums to bandwith and quality compromises – as well as being unreproducible in real-world combinations of colour, lighting, lighting colour, angle, viewing setup (including colour space, compression, viewing environment, monitor seup and colour space, etc…)
And if you think that doesn’t sound right, there’s a reason the surgical consultant often gets the last call on removing the appendix, and often makes that call based on their own clinical examination (yes, despite the availiability or findings of ultrasound);
They’re good at it. And to make anyone else that good would be making them a general surgeon.
The last is tackling cost vs. distance. I’m told that earlier this century, Papua New Ginuea (a former British empire conquest and briefly under the govenance of Australia, now destitute and pillaged by internaional companies and its own peoples) had an annual health budget per person of US$1. Snake envenomation (read: bite) was one of the major contributors to non-infant mortality and the rate of mortality was around 10% they reached Port Moresby’s (The capital city) ICU and contributed about 50% of the patients needing intensive care (much of the rest was vehicle accidents).
Less than 60% of those who died had recieved antivenom; only 5% within 4 hours of the bite, and mostly a single dose (where an envenomation in Australia might recieve up to 20 doses.
Why? Because a single dose of antivenom cost rose to around A$2000 (at least 1.5x the gross domestic product per capita, or average total income per person per year, in PNG). Because it was 40x more expensive in terms of GDP in PNG than it was in Australia. Because they used all they could afford and get their hands on. Because they were a long way away from the point of care and even further from the point of manufacture, and when they arrived at outlying care centers none of the (short shelf life, expensive) product was available.
(They also died while relatives had to hand ventilate their loved ones, because the medical gas cut out, and generally because they places the largest burdin on the ICU of any other diagnosis)
But largely they missed out because they couldn’t afford it (Because of the floating of the Kina and the lack of domestic manufacture). Or they couldn’t afford to provided it far from the population base (i.e. everywhere outside port moresby) because of the poor shelf life, or private individuales purchasing supply.
So fix these issues:
– Acceptability of the remote clinician
– Ability to tele-examine patients wit the same or similar fidelity as in person
– Be able to afford the intervention, and affording meaning transportation costs of the therapy, the patient and of course the teletechnology in the first place.
I would, however, love to work with someone who could help put together a service that
– Allows roaming midwives to diagnose pregnancy and give appropriate (modern) birthing advise to remote community women
– Schedule an automatic delivery of a “birth kit” (clean toweling, clean water, clean scissors, an umbilical cord clamp and a shot of misoprol or equiv.) just before birth, via drone, or;
– Provide an epirb-like device capable of long-distance commuication about an impending birth or complication, notifying the health worker / midwife in the district and potentially send the aforementioned birthing kit +/- a basic telepresence unit to the site via drone
– Allowing the health worker to be notified of the birth as soon as possible, or the labour if in a woman identified as needing to go to hospital for safe birth, or to inspect the child after birth.
Low-cost EPIRB like module for notifying of confirmed Labor
Low cost, possible unrecoverable telepresence drone
Long-distance delivery of birthing packs (probably via drone)
Something like Barefoot Doctors with Appropriate Technology medical gear?
http://en.wikipedia.org/wiki/Barefoot_doctor
I spent 2.5 years riding a bicycle through South and Central America. Wrote a book about it too.
http://davesnewadventure.com
And during the process, I did some side volunteer consulting work with the Peace Corps. In the most remotest places of the Amazon, or the Peten, or the Altiplano, I always found these guides with the Peace Corps workers out there. “Where there is no Doctor”, and “Where there is no Dentist.” They’re the go to guides for medicine in the most remote of remotes. I can tell you right now, being a vet of some of the most isolated places on the planet, that a technological solution is at best a band aid, based on my experiences out there. You know what it’s like to go for months without internet? Or electricity? Or running water? I do.
That said, I did find some interesting anachronisms out there. I was in the sticks, Amazon, in a village of what, 80 people, and there was a dinky little building with a satellite dish and and some computers. I emailed my folks from there for 15 bolivianos’ per hour. That’s two bucks, and that’s very expensive for that area.
Anything you build has got to have the smallest, tiniest data rate, if you want to communicate online. The bulk of what you’ll need down there has to be able to run with little to no outside support. No cloud’s honey. It has to be built to endure extreme heat, humidity, and take static shock like nobody’s business. Replacement parts are scarce, period. It has to be cheap, and run off commonly available supplies. And it has to be USEFUL, as in better than the periodically roving field doctor’s stethescope. What’s the point of trying to sell a glorified 90 dollar fitbit as a health monitor when your average campesino makes that much in 3 months?
Riding my bicycle through Latin America was a life changer for me, and it opened my eyes up to being in touch with poverty, and what people really need. I highly recommend that if you ever have a slight feeling to volunteer in a very poor, impoverished third world country, go do it. Your soul will open up.
Don’t let my write up about what I’ve learned discourage you. I’m trying to figure it our myself with my tech. But be honest about your ignorance to the poor’s human condition. That’s all I ask.
Doctors are repositories of knowledge and experience with a set of hands and legs attached. For some reason the focus has been on extending those hands and legs through robots and telepresence, when what the poor really need is the knowledge.
We need a good app with step by step diagnosis and treatment walkthroughs. Throw in some adaptive algorithms so we can actually improve medical treatment and you have a winner. I’m not a mechanic but I can change my brakes with a youtube walkthrough. Focusing on hydration, administering solutes, administering vaccines, keeping down a fever and basic hygiene aren’t rocket science, but when you’ve lived in an isolated and poor village all your life you don’t know any better. Get the knowledge to mothers so they can treat their children and at the same time gather data to better distribute the meagre resources available.
To whoever develops the app: hire lawyers, many, many lawyers…
The app doesn’t exist because the diagnosis doesn’t get easily broken down to elements that are easily model label.
Take the example of a sore throat, red throat and 24 hour onset. It’s probably a virus (in a western community). You should probably rest. It’s >80% likely to be one of five or six viruses with no antiviral agent
But sometimes it’s bacterial
Sometimes it’s streptococcus and sometimes you’re going to get rheumatic fever.
These options are unlikely and hard to pick; you have to be able to differentiate qualitative findings that cross an individual case from the 80% to the 20%.
Believe it or not we do have guidelines that try this; problem is that we’re not great at following them, and patients hate them (it is normal to want to be treated as a special case and to be concerned that you have the rarity not the normality)
Plus the course of action changes with the type of patient. A healthy 25 yo will need to rest, while the 80 yo in hospice care taking immuno suppressive medications for her arthritis will likely need further evaluation and care. And if she need some antibiotics it’s likely different than the antibiotics a 2 yo with the same condition might need.
So basically, if the app existed, it would need a huge amount of resources to keep it complete and up to date, not to mention reconciliation of all the conflicting recommendations that exist. Including trying to include and interpret the limited available data for the remote places its intended to he used in.
In the end it would be so complex of an app, you’d probably need to be a doctor to use it properly.
There are a finite number of symptoms and a finite number of causes. It is impossible, with current computing power, that a doctor is more efficient at making a diagnosis than a computer. From manufacturing, to driving cars, to identifying cancer cells computers are superior to human beings.
Customizing diagnosis to geographical regions and patient history is exactly the sort of application big data is best at.
It’s a lack of education really. All the places that you speak of have their own problems with education, or a lack there of, to the point a lot of it boils down to superstitions and fear of the unknown (is this a life saving electronic device or a tool of the devil?) Sounds silly, but it’s true.
So putting AED’s in the middle of a jungle village sounds wonderful and all, but actually getting someone to use it is hard enough, even when educated (a lot of people die awaiting care such as CPR because the people around them are paralyzed with fear, people that have CPR training in fact) let alone getting them to not be afraid of some very foreign thing they may well view as black magic.
Even with AEDs, someone has to attach the device to the patient, and people have a funny way of failing to keep their wits in such situations.
So just educating some people not to be afraid to step in and help with basic care is hard enough, now you want to include technology where technology is viewed as the work of evil? Good luck…
Even when people are *supposedly* educated, some of them would do the irrational things because of personal belief or just plain ignorance. See the recent movement of people against immunization and see how that cause infectious diseases on to others. Don’t get me started on the unproven “alternative” medical treatments for critical diseases.
Oh please do get started, maybe you should focus on all the side effects of western “medicine” and psychiatry drugs. You are a cultist but you can’t see it, a healthy doubt of both methodology is in order. You seriously can’t believe that over vaccination and over administration of anti-biotics will really help humanity 100 years down the road. There have been numerous cases of people being vaccinated and still aquiring viral disease.
Please get started on cannibinoids as well as not being effective as initiating apoptosis in cancer cells. The US government recently admitted brain tumors shrink and dissapear when the patient is administered cbd’s. But yet cannabis remains a schedule 1 drug. The antihelmintic medicine mebendazole has been proven effective against cancer but is no longer made as the patent has expired and there is less money to be made off it over patented chemo drugs. You need to seriously reconsider your religion of blind faith in western medicine.
Read carefully… I specifically said: unproven “alternative” medical treatments.
Until you use *proper* scientific method e.g. double blind test and fully understand the mechanisms (biology, chemistry etc) behind how/why/how much it works, it is unproven. You don’t even know my cultural background to say it is “western” medicine. I specifically didn’t specify whart type of medicine. You already formed a bias without knowing.
Not saying that *all* alternative medicine are bad, just that there are too many out there that have not been proven. There are tons of the historical folk medicine that are proven and are recognized and there are also a large number of them that are totally ineffective.
So basically your comment was an infallible vague argument, wow you are a complete brainiac or just a troll.
So let me get this straight… if something is unproven it is ineffective? Yep still brainwashed, by your logic the garlic, bile treatment for eye infections known for thousands of years by northern europeans was innefective untill recently tested and “proven.”
If something works it works, it doesn’t need to be proven by a bunch of jerkoffs in white coats who pay sole homage to establishment, and then recorded in your holy peer reviewed scientific journal by the prophets of your infallible religion. Why not join a christian church or the muslim brotherhood while you are blindly following others?
Go back to reddit please we all beg you no need for your circle jerking hivemind lunacy here.
Somehow, within your first few sentences I just KNEW you were a pothead.
So why do you suppose there aren’t a lot of healthcare workers? I bet if you think real hard, you can figure it out.
Actually there are a lot of reasons. Historically, health care training has focused on creating doctors. This is actually a poor model, as the biggest improvements in overall health are obtained from the kind of public health and prophylactic care that is more efficiently provided by nurses, midwives, etc. These are traditionally female jobs and therefor historically undervalued. (Doctors are seen as prestigious/valuable independently, so there is a double whammey effect for training fewer nurses) Also Hospitals (as with doctors) are visible and valued(by governments AND donors) where as more effective dispersed clinics and independent workers are neither. Centralized Hospital/Doctor medical systems are also easier to control and provide great leverage for authoritarian governments. Finally while training a doctor is much more expensive and time consuming than training a village health worker, nurse or midwife, the doctor is likely to emmigrate to somewhere where his skills command a much higher price, the others are less motivated because the pay differential is less. Doctors see patients from all over who are sick whereas healthcare workers live in the community and provide well care as well as sick care. Thgird world educational systems tend to be elitist and top heavy, producing a few college graduates rather than a broad base of literate technical workers. Again the reasons are historical/colonial, political and economic. So yes I can figure it out, it’s just not easy to solve.
You really are naive. First the single best means of improving health of the worlds population is the provision of proper nutrition and the elimination of bad habits. That said, you really can’t do that if you allow people individual choice… So after accusing me of being a sociopath are you willing to admit your personal fashism?
Second, ANY group trained with useful skills will tend to relocate to where those skills provide them their maximum value… Not just doctors…
If anyone has the time, please join the US Peace Corps and spend some time in a region that needs help (or an aid organization that is spending on technology and not slickly produced solicitation videos). It will give you insight into what problems on the ground are. Poor infrastructure that retards response time, not enough basic equipment, inadequate sanitation, doctors and healthcare workers working on pennies because the state or their patients are literally dirt poor, etc. If you make telepresence or dissemination of knowledge easier, you still need somebody at the other end with the technical training to carry out procedures while also having the proper equipment and, in many cases, electricity for more sophisticated equipment. Cheaper, more portable, easily deployable power generation would be nice but the easier and higher value things are to carry around the more attractive they are for thieves and bandits as well.
+1 to this. I did a long tour down there. Just posted about it above. Understand what the poor go through first before thinking about technological solutions. Not the other way around.
here is one that might work in the us: build a flame throwing robot to burn all the bureaucracy. you might also throw on a machine gun to hunt out malpractice attorneys.
Sorry to create a boogeyman from malpractice lawsuits, is merely bullshit used to prevent the ignorant from taking look around to figure out what are the real problems with health care in the US. train your weaponry on those who are in healthcare to earn a profit only, not to provide actual care. Hint; just wages for those actually providing the care isn’t profit. The idea that investors are to be protected at all costs is insane & natural. Business have always failed from time to time. Yea tough when it happens to your business, but it’s a risk many take anyway, because the potential rewards are much greater than any losses
How about training all of the illegal immigrants who come to the U.S. to be medics that can the be sent back to their home country? We could call it the U.S. Envoy Program. They come in, we train them, we sent them home (with maybe a bit of security of other illegal immigrants trained for security), and then, they could actually get to work to improve their own country. They don’t have to be trained to be experts in medicine (or security), just enough to start the process towards doing better. I know that we already have international students that roll through here on student visas and return home when they’re done with their education, but there really isn’t enough of them to effectively create much change for the better for their home country (or rather, not enough from the countries that really need the help).
To even start this right, we would have to focus our efforts towards allowing the illegal immigrants to be able to learn the simplest form of education with the particular field of choice. Remember, they don’t have to be experts, they just need to get the simplest of train because even the bear minimum will effect huge change. If we can make it cheap for these people to learn how to do this, while also teaching them how to be resourceful enough to use what’s local to their home country to use for medication, they would be better equipped to get the job done. Plus, they would need less from everyone else in terms of equipment. Even better would be if they successfully setup a new business or industry in there though it would not be necessarily required.
I’m sure someone would think “Who going to pay for all of this?” To be honest, I really hate that question. Not that it isn’t a valid question to ask, it does need to be asked. What I hate about that question is that it is used to inhibit programs that are need to help improve quality of life. Put simply, if illegal immigration is cost the U.S. so much money, wouldn’t it be cheaper to train them so that they can improve their own country instead of just sending them back to the place that they was trying to escape from because condition in their country is so bad?
Aside from that, those countries that are a bit of ways out of range (African countries and in the South Pacific), maybe setting up schools that do the same in those countries might work as well. Make cheap nursing schools, security schools and so forth. Again, they don’t have to be experts. Training them to be experts would cost too much and take too long. Maybe we could “hack” together a training program to help. A hacked together school is better than none at all.
Sorry for the long post with the political slant.
You like your bogeymen, eh? A decent plan, but on that those who make money from the illegal labor wouldn’t like. Would anyone really believe that those ho use illegal labor send the taxes the deduct from the lower wage actually goes to the designated agencies? All of our bank accounts the labor(legal and/or illegal) doing the work that the illegal labor is doing is paid a just wage
You’re probably better off contacting and partnering with an organization like Partners in Health (http://www.pih.org). I helped them with web hosting many many moons ago. Their idea was to have doctors or volunteers in remote areas, then upload the data they collected to volunteers in the US who would be able to interpret the data and make a diagnosis. So an X-Ray in Haiti would be sent to Boston for analysis. Time consuming, but the volunteers in Boston don’t need to go anywhere, which probably increases the volunteer workforce as they could review X-Rays from multiple locations without leaving town. They took some action after the Haiti earthquake and also sent a team to West Africa for the Ebola outbreak.
While I’m sure there’s great ideas out there, whipping up an AED using an Arduino and a car battery would be awesome, but somewhat impractical to take into the field especially if there’s different designs that work in different manners. That being said, if HAD was able to come up with prototypes and collaborate with PIH or SWF to make equipment that could consistently work and could be made really inexpensively, that would be great for everyone. Sorry if I sound like a debbie downer on this.
As an MD and an MEng (electrical engineering) in a 1st world country (The Netherlands) I have been asking myself similar questions during the last decade and a half. There are two parts to the problem: diagnosis and intervention/treatment.
Creating a differential diagnosis is often considered an art that requires a skill set honed by experience in asking the right questions and performing a proper physical examination, if necessary complemented by various types of more or less costly tests. Most of those tests are used to reduce uncertainty and basically demonstrate what the physician already suspected.
Mind you, this is not a simple process. It requires deep knowledge of disease patterns and symptoms and of correlations between them. Basically, it requires the ability to build a mental model of a person and her possible disease and the ability to use the process described above to arrive at one or more models that are consistent with both experience/training and the specific patient data obtained.
Typically, at least in my country, clinical decision support systems are rarely used in daily practice. Perhaps they could have been built into our electronic health record systems, but they weren’t. A system like IBM’s Watson could reduce the need for highly specialized healthcare professionals in creating differential diagnoses, but such systems are not (yet) part of ordinary healthcare.
A given differential diagnosis leads to the question, what intervention should be used. There is a scientific and a practical side to that question. The scientific question relates to the amount and quality of evidence available for the various interventions that could alleviate the patient’s problems (or sometimes merely its symptoms) given a certain diagnosis. Once an intervention has been chosen and implemented, its results can produce information that may alter the differential diagnosis. Once again, in theory clinical decision support systems could be very helpful in this complicated process, but they are not (commonly) used.
Of course, there is also a practical side to medical intervention. It requires resources and sometimes (hand) skill that is not always readily available. Some of these problemens may be solved by 3D printers and local production of drugs like antibiotics and pain killers, or even science-driven use of medicinal plants. As detailed in earlier posts above, there are problems like poor drinking water quality that require political and economical change, given the fact that technology to solve these problems is readily available but is still out of reach for billions of people.
To conclude: the medical process of diagnosis and treatment depends critically on a load of information. Putting that information into the hands of patients, their caretakers and non-specialist health workers would make medical care much more accessible. It would require clinical decision support systems like IBM’s Watson to be much more widely available.
“The doctor of the future will give no medicine, but will educate his patients in the care of the human frame, in diet, and in the cause and prevention of disease.” — Thomas Edison
Excellent post.
Well explained about the “mental model” of the physiology and pathology.
There remains great scope for automated not-quite-big data analysis well before it gets to the doctor
Eg. “The patients bilirubin is high. Note that this is not new and that other tests are not detanged today/this occurs roughly every 6 months / were previously normal would you like to retest?. The patient has a liver ultrasound on file that is normal / that shows a minor abnormality. Review?
I believe that this technology can save even more lives than the AED does: fire.
In particular, using fire to boil water.
A few medical use cases for areas with shortages of institutionally certified medicine mamas:
Get water, and boil the water before use, wash hands and wounds with boiled water (after it cools below scalding). Wash hands after caring for sick relatives, and wash hands between caring for different sick people. Wash hands with boiled water before cooking or eating. Don’t put clothing from sick people on anyone else until it is cleaned in boiling water (while it is boiling).
Not as “medicine” like, but still helpful: drink only water that has been boiled, and wash vegetables (and hands) with boiled water before eating. Only allow healthy people to cook meals and wash vegetables. Don’t put poop from sick people on the garden.
This is limited by a couple of things, though. Ability to get water. Energy/fuel to boil water. Those are still big limiting problems to the application of this particular technology.
Automatic External Defibrillators are great devices for first aid. Helping people in emergencies is great, but not the only way to improve their lives. Here are my thoughts of possible categories:
1) First Aid Devices
Devices for helping people in an emergency. Possible things would be accidents, heart attacks etc.
2) Telemedicine
Share Informations of the patient live to a doctor somewhere else.
3) Information for the untrained
Devices which provide information on the disease/injury of the patient.
4) Devices for treatment
Devices which can actually treat the patient.
Here some thoughts:
– If people get sick they might think visiting a doctor. If the next hosptial is 100 km away, the patient will think twice going there. A trip can be expensive and if the disease is not really treatable or will go away on its own, the patient will just pay for nothing. This means people will wait to the last moment when the disease is already really bad. If we could tell the patient reliable if he/she should visit a hospital or not, we might help them.
– Sometimes its obvious what treatment is necessary. If a person is bitten by a known snake, the person needs to get injections of antivenom. An injection could be done by an untrained, but antivenoms are expensive and can’t be stored in every small village. How about a fast delivery system? I was thinking of small drones delivering this by GPS coordinates / parachute.
Some food for thought, or at least some background on others who have contemplated, if not investigated these very issues. Others have started down this path before you, so I would recommend to anyone serious to actually save themselves a large effort of wasted time and efforts and learn from others have travelled this road before you. For those interested primarily in knee-jerk pontification, feel free to ignore.
This is a complex and difficult subject, I’ve included a short list of articles from a single (freely available online) electronic engineering magazine (IEEE Spectrum) that I recall from the last few years.
AED:
The Shocking Truth About Defibrillators
http://spectrum.ieee.org/biomedical/devices/the-shocking-truth-about-defibrillators
A 911 Registry for AEDs
http://spectrum.ieee.org/tech-talk/biomedical/devices/a-911-registry-for-aeds
Telemedicine:
Review: The Edge of Medicine
http://spectrum.ieee.org/biomedical/diagnostics/the-edge-of-medicine
Mobile medicine:
Medtronic Sees a High-Tech Solution to Global Health Woes
http://spectrum.ieee.org/tech-talk/biomedical/devices/medtronic-sees-a-hightech-solution-to-global-health-woes
Robert Malkin: MacGyvering Medical Gear
http://spectrum.ieee.org/biomedical/devices/robert-malkin-macgyvering-medical-gear
Security (and privacy):
Feds Probe Cybersecurity Dangers in Medical Devices
http://spectrum.ieee.org/tech-talk/biomedical/devices/feds-probe-cybersecurity-dangers-in-medical-devices
Q&A With Bioengineer Tejal Desai
http://spectrum.ieee.org/biomedical/diagnostics/qa-with-bioengineer-tejal-desai
I spent a long time in the worst parts of Latin America. You know what would improve their health and well being? In this order it is:
Access to cheap energy
Clean water and sanitation
Free markets that generate paying jobs
Education
Women’s rights
After 2.5 years of time there, that’s what I’ve learned. Solve those issues, and you’ll have health and mortality rates sky rocket to 1st world levels. You’ll have full on population stabilization to 1st world rates of 1.3 per couple.
I’d say most of the diseases and problems I ran into down there, are preventable. And when I mean prevention, I mean the worst killers which come from the lack of sanitation and clean water. One of the greatest technological movements going on today in the world is bringing a better toilet.
That’s right, a better way to remove your number 1 and 2. That alone will save more lives, and improve more conditions, than any vaccine, surgery, drug, robot dohickey, internet app whiz bang machine, you name it.
Solve sanitation, and you’ve solved most of the problems…
Don’t we already have bacterial compounds used in portable toilets, planes, and RVs that literally eat the excrement and create a safe byproduct? Or am I imagining things?
Several have touched on this, but I don’t think it has gotten the point across well enough. Prevention. Many of the ideas, and the article itself focuses on emergency response, an after-the-fact fix. So what can we do with technology (that does not mean electronics exclusively) to aid in prevention? How can we use technology to educate, support, and re-enforce good hygeine, diet, etc…? Simply telling someone to wash their hands several times a day and before doing things that might spread a bacteria or virus is not enough because the cause-affect is not immediately visible. People cannot see viruses and bacteria on their hands. They don’t always become sick when they don’t wash their hands. Even in a 1st world country like the U.S. many people don’t wash their hands after using the bathroom, before cooking, after handling raw meat and eggs. Many people don’t even wash their produce. Yet they KNOW they should. But they cut these corners simply because 9/10 they see no ill effect to not doing so and even in that 1/10 case they completely miss the action as the cause.
So what can we do about that? It sounds less heroic than pulling someone back from the brink of death, but IMO better to prevent them from ever reaching the brink of death in the first place.
Let’s take an idea from Star Trek and local hospitals today. US hospitals have been using Skype to do off-shore outsourcing of medical diagnosticians. Local US doctors use Indian doctors in Bangalore India by “picking their brains” via Skype. The Indian outsourcer gets to meet the patient and ask questions, The local doctor or nurse or P.A. can physically administer whatever medical recommendations he/she makes.
This idea can be evolved one step further for remote areas of the world with little or no doctors. Nurses, or very well medical trained civilians, could be supplied with fully vetted emergency and sundry medical supplies and a satellite data terminal(s) with laptop with Skype on it. Some areas already have Internet access (i.e. internet cafes, public libraries, etc.). A triage tent could be set up at these locations and patients could sit (or lay) in front of the Skype terminal(s). The local nurse or med technician could follow whatever instructions given by the remote doctor. Obviously major medical procedures would involve MEDEVAC to closest hospital.
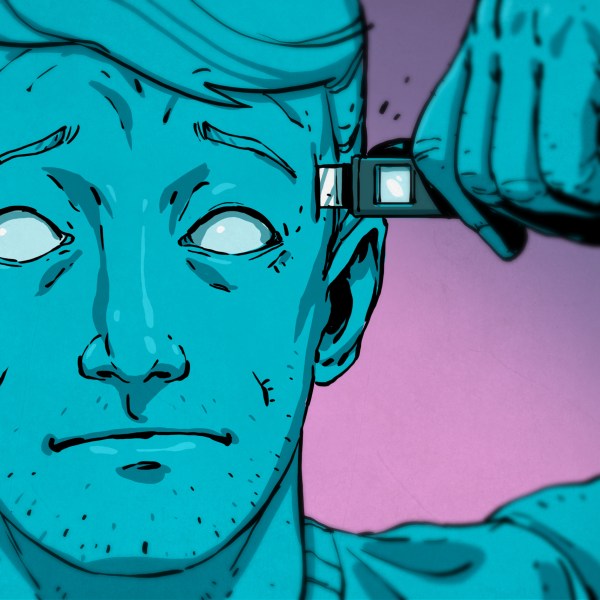
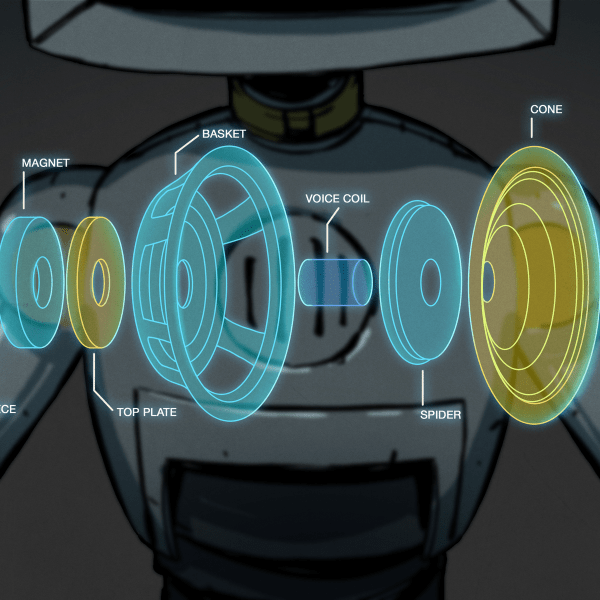
Where does Star Trek and HaD come in? Remember the Star Trek TRICORDER that the ship’s surgeon uses? HaD could design and build one for this project. It is basically a multiple human body sensor monitor that attaches to Skype via video or automated file transfer. Two separate Skype terminals should be used. One for Tricorder functions and one for face-to-face consultation for patient and local medical technician. The Tricorder terminal needs to have a tech make labels in ENGLISH labeling what the remote doctor is looking at (i.e. Blood Pressure, Heart Rate, EEG, etc.)
Here is a list of human body functions that can be easily monitored with existing (or surplus) cheap toy electronics – and other stuff too:
1) EEG – Remember the Mind Control toys with the 2.4 Ghz head piece? They monitor brain waves.This will need some R&D to figure out how to display Alpha, Theta, and Delta waves.Audio doesn’t seem detailed enough. Some sort of oscilloscope or graphing function is needed here.
2) EKG – a simple skin resistance sensor and DC amplifier which could send pulse rate to Skype.Cannibalize a wrist watch heart rate monitor. Aim Skype webcam at wrist watch attached to patient’s arm. Clean skin with alcohol wipe and wipe on some sort of conductive cream or liquid to enhance sensor sensitivity. Leaving this attached to patient during examination is indicated. That way you can monitor EKG constantly. #5 can be used to check calibration.
3) Respiration sensor – a sort of stretch sensor (i.e. strain gauge) that wraps around patient’s chest and changes resistance base on patients breathing rate. Cannibalize a wrist watch heart rate monitor with remote chest respiratory sensor.
4) Toy camera microscope ([i.e. Jakks EyeClops Bionic Eye) that could be used for eye, ear, and throat examination device (i.e. otoscope). Video out goes to video capture module or just point Skype webcam at EyeClops TV monitor. EyeClops has it’s own illumination LED. But you could build in a better one. Also the chassis is stupid looking (big eyeball). Maybe a new style cool looking case. This device could also be used to visually examine body fluid microscopically. They have amazing magnification powers. Finding a way to mounting it on a tripod wouldn’t hurt either.
5) Blood Pressure monitor – use a cheap battery operated automated BP monitor and aim Skype webcam at LCD display. Make sure patient’s arm is resting on a table and use fresh alkaline batteries. An AC power supply would be better than batteries. They kind that has a remote display AWAY from the cuff would be indicated here for this project. That way you could Velcro the display in front of the Skype webcam away from patient moving around.
6) Electronic stethoscope – get a cheap prenatal baby heart rate monitor and plug audio audio output to Skype Tricorder terminal microphone input. Or just point microphone at the stethoscope’s earpiece.
7) Blood Sugar monitor – These are readily available everywhere. The medical tech would take blood sample and put the strip it he device for analysis. Just aim the Skype webcam at the unit’s LCD display. This should only be done when remote doctor asks for this so as not to confuse patient strips,
8) A cheap LCD clock that displays local time and date. A separate one that displays remote doctor’s local time and date. Also another for GMT (UTC or Zulu), This is critical believe it or not. Time log is very important in medicine. Always replace batteries periodically.
9) A separate Internet laptop or PC attached to a automated medical diagnostic program in case remote doctor not available or lost link. Also is good for 2nd opinion type consultation. Just remember to have remote doctors to check their egos at the door (i.e. be tolerant) when you use #9 in front of them.
10) AED – make sure batteries are always fresh or recharged. Every user must be trained in it’s use. They are available surplus and under government grants.
11) Remote pain indicator – A strain gauge attached to a hand exerciser that indicates a scale of 0 to 10. Tell patient that 0 means no pain at all or not squeezing it at all, 5 means moderate pain. 10 means really bad pain the worse. It could be LCD digital or a analog VU meter. Patient doesn’t have to vocalize pain just squeeze hand controller. He/She could constantly watch display to indicate pain during examination. If they can’t use hands or are blind then #11 is pointless. 10 should set off a audio beeper too to alert med tech if he isn’t paying close attention already.
12) VSA – voice stress analysis – usually this is used for lie detection. However, you can use this to detect stress or deception. This can be downloaded for free or use the Israeli made TRUSTER. Just get a baseline (patient’s name and particulars) then everything they say afterwards is with or without stress.
13) Snake inspection camera – these are very cheap now (i.e. Harbor Freight). They have a thin illuminated snake like camera head and a LCD video monitor with JPG file saving ability via USB port. Of course it will need to be sterilized with hand sanitizer or alcohol before you stick it in a human orifice. Don’t stick it wounds – too tight and will aggravate wound. Also it wont work well with Vaseline on camera either. Not recommended as a proctologist tool. Since you cant put Vaseline on a camera, you can’t cover with plastic and expect to see anything, and if you don’t have patient do a colorectal cleansing ahead of time you can see how this one wont work well for proctologist exam. However, it works great for 1st responder emergency building tight space survival examination for earthquake or building collapse victims. You can also physically exam a patient stuck in a building or structure collapse. This would make a great replacement for #4 but it doesn’t magnify nor does it have video output. Makes for great dental exam tool.
14) Tons of Hand Sanitizer – local med techs should use this RELIGIOUSLY to avoid cross contamination and infectious disease transmittal from patient to patient (and themselves), This stuff is great for sanitizing toilet seats and bowl before use. Always carry a small bottle in your pocket just in case. However, still wash your hands constantly. Don’t depend on this stuff to clean your hands totally.
15) Catheter (male) – Benjamin Franklin designed one for his cousin that was much more comfortable for him. Sometimes due to male genitalia it is difficult to do urethra catheterizing. Sometimes difficult to do urine samples too. A method to guide urine away from body into a receptacle (empty milk jug?) without using invasive and painful urethra insertion. One idea is to use an over genital catheter. Using a small section of PVC vacuum cleaner hose (the stiff part leading up to the hose). Hacksaw a 1 to 2-foot section. Always wash it it out with scalding hot water after use and put #14 around the inside and outside of tip that touches the human. This is for emergencies only. It keeps patient’s clothing unsoiled and can be aimed on right angles. Patient (or nurse) just needs to put it on (one size MOSTLY fits all sizes). Easily concealable too. Black hose pipes work great at night when patient needs to go outside in the woods. Just remember SANITIZE SANITIZE SANITIZE!
16) Thermometer – Life Labs Wireless Remote Thermometer Temperature Monitoring System – uses 2.4 Ghz. Battery operated. Very cheap from China. About $20 USD. On EBAY right now.
17) Google Translate with voice to text – need for this is obvious and it’s free. You can actually have patient speak in his/her native language and Google will generally translate it to English. Works vice versa too. This is great for 1st responders in foreign lands. Works better on SMARTPHONE but can also work on PC tablet or laptop.
18) A basic patient interview questionnaire which asks all of the pertinent questions the remote doctor will ask. So get it done ahead of time. A automated computer program would be better. It would save to a remote database and doctor can view it by ID number. All Tricorder readings should be performed and entered before doctor is brought up online.
19) Tons of Nitrile rubber gloves. Self explanatory. In an emergency use a plastic bag with a rubber hand to hold it on your hands or it will slip off. Baggies, grocery bag, newspaper bag, etc.
20) Believe it or not Radio Shack sells scalpels. Just remember to sterilize it thoroughly and only use it under the remote doctor’s assistance. Some people do their own sebaceous cyst excisions but NOT recommended at al!!
Maybe you can add to this list?
#15 – is TAPERED and can be cut to conform to girth. Just remember to debur it and use sandpaper to make it painless to patient. Let patient keep it as their personal one. But you could have a communal one if you practice intense sterilization procedures on it. I have nothing in mind for females. Maybe somebody else cam tackle that one.
The TRICORDER display should be mounted vertically on a wooden board on the wall for patient and med tech to view easily. Then the Skype webcam can be mounted on a tripod and aimed at it for remote doctor. BIG large font black on white labels should label all displays on the board. Some sort of illumination is needed for the LCD displays and the webcam. Nobody should walk or stand there so as not to block doctor’s view of Tricorder board. The webcam can be moved to aim at other stuff like the BP/Pulse wrist watch unless you can figure out a remote display for that.All small TV video monitor can be mounted on Tricorder board for the othoscope EyeClops Bionic eye.
I know someone can figure out how to use an Arduino or Rasberry Pi for this.
I live in Quebec. We have no doctors here either… or at least it feels like that is the case