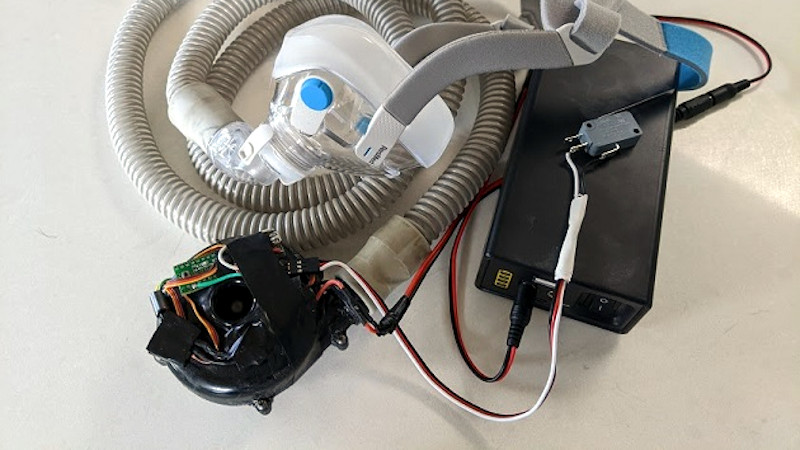
Watching the hardware community respond to the global pandemic is a fascinating process, because of the breadth of projects being considered, and also because of the differing experiences and perspectives being brought to the table. Components most of us might have been unaware of are appearing, such as the CPAP blower used by [Jcl5m1] in his ventilator design.
He starts with a very necessary disclaimer against trusting a random person on the Internet on the subject of medical equipment design, and since it must be possible to do damage with an inappropriate ventilator we can only echo that. But as a CPAP user he’s familiar with their operation and parts, and he’s taken the centrifugal blower from one of them and paired it with a speed controller and an Arduino to provide an adjustable pressure.
What we take away from this is not in any way a ventilator that’s ready to be hooked up to sick patients, but an interesting look at ventilators in general, CPAP components, and the possibility that this project and others like it might eventually form the basis of something more useful if they attract the attention of people with more experience in the field. We’ve already seen 3D-printing used to make valves for a respirator at a hospital in Italy.













International group of volunteers for trying to help with this:
https://www.projectopenair.org/
It is possible to use some CPAP/BiPAP/APAP machines as ventilators and connect them to oxygen supplies. You may be aware of this already, but there are a lot of CPAP machines available for not a lot of money that could be used to augment full hospital-grade ventilators. I’m sure others with much more expertise have already thought of this but if UPenn is not already using these, it might be a good time now to investigate and get logistics started for use when the peak comes. You do not have to open up the CPAP machine, just program it. BiPAP mode can be used though it may not be optimum.
Below is a medical research paper I found on the topic from 2010, I think:
https://acphospitalist.org/archives/2010/09/tech.htm
Here is another resource
https://emcrit.org/pulmcrit/cpap-covid/
I see three things hackers might be able to help a lot with.
1. The parameters of consumer CPAP machines sold for home use are typically set once in an office visit with a doctor. Creating a better interface for modifying these parameters in an intensive-care setting may be necessary. The standard OEM software for this purpose may be hard to obtain and likely inadequate.
2. In CPAP mode ICU ventilators provide a live feedback from sensors of tidal volume and minute ventilation which are clinically useful in accessing the effectiveness of treatment and when a patient needs to be moved to more intensive therapies. Adding that kind of feature to consumer CPAP machines could save lives.
3. Helmet interfaces (basically a big clear diving helmet) seem to have many advantages with ICU CPAP but are rare. They look like something which could be improvised with some effort, and figuring out how to make one reliably might be very useful.
AVAPs would be the mode to switch standard Bipap machines to.
Here is the full explanation of ventilator functioning
https://www.youtube.com/watch?v=gk_Qf-JAL84&feature=youtu.be&fbclid=IwAR0uk0pMLIUxSvEKYlhAWKHb_MgaLH4IJlwOhmcYNzVHN4ZttS1diX6cnXw
How to Make an Oxy Ventilator in 10 minutes:
I have a Resmed CPAP with automatic pressure adjustment up to 20cm. 20cm is considered nearly full ventilation -total ventilation is 30cm. 20cm would be enough for most people needing ventilation. And there are portable oxygen generators. So how to combine them fast?
My hacker idea: Get a 5 gallon bucket with a lid – a Home Depot Homer bucket is perfect. Put your CPAP in the bucket. Make two holes in the side of the bucket. One of them should be just big enough to get the CPAP mask hose thru it. Put the oxygen generator next to the bucket. Make the other hole in the side big enough to insert the oxygen output hose. In the bucket lid, cut a slot in the rim about an inch long in from the edge, including the lip. Put the CPAP power cord thru that slit and put the lid on the bucket. Plug both machines and turn on. Now the oxygen generator is filling the bucket with nearly pure oxy, and the CPAP is pulling that in and pushing it out to the mask. The auto CPAP already is adjusting its pressure depending on how many apnea events I have (more means raise the pressure). Adjusting on the fly should be possible. It sure would be better than suffocating without any ventilator.
I thought the same thing, only if used in hospital setting, configure a hose to the input to the pump, and connect to the regulatable humidified oxygen source that is already available in every single hospital room.
I like the idea/concept. I’ve been thinking about this for a few nights now.
Please don’t try this! First, 100% oxygen is almost always fatal! Using this method the only source of gas for the cpap is from the concentrator (100% oxygen). Even then, most cpaps will try to deliver much more volume than the concentrator can provide, resulting in a vacuum in the bucket, and not enough flow for the patient. Most medical supply houses sell a small plastic unit that fits into the cpap hose and allows an oxygen tube to be connected, thereby allowing a titrated flow of oxygen into the delivered air. This is a much better situation.
Oxygen concentrators don’t put out 100% oxygen. This is why they don’t kill people in hospitals when connections them to ventilators.
I had a CPAP combined with a concentrator which was tapped into the hose from the CPAP and it worked for me and have been asking myself if this would work as a ventilator substitute
Yes, I agree. This would be safer and very convenient to apply.
This sounds very dangerous.. filling a bucket with pure oxygen?.. sounds like a bomb.. and an electrical motor to provide the spark..
Oxygen is not flamable. It can make flames burn hotter.
Operating any electrical device in a high oxygen environment will create a serious fire hazard. Oxygen + plastic + spark from switch contacts or motor brushes will likely create an ugly fast fire. Don’t do that.
Not a bomb but the motor may catch fire and spread out and the whole bucket on fire. Almost pure oxygen is a very good oxidative.
Oxygen is not flammable. It’s an accelerant
The CPAP has a water reservoir, I guess it must suck the air in somewhere, and use the water to regulate the temperature of the air flow.
Where does one get an oxygen pump from? And oxygen tanks for that matter. How long does one tank last?
There are oxygen enrichment modifications that can be made to increase the oxygen supply in the cpap without doing all of the stuff here – suggest you look at this hose which works with the ResMed Airsense 10 – https://www.cpap.com/productpage/resmed-climatelineair-oxy-tube-airsense-aircurve-10. Less fatal :). There are most likely equivalent hoses that are available for other cpaps.
Need a prescription for both of these items
I took my CPAP to the hospital as I was staying overnight following surgery. They tested it for correct pressure and put an insert in the tube that introduced regulated oxygen from the hospital system.
I personally would be a bit more hesitant to introduce an electric motor into an oxygenated environment whithout doing some research to determine if it is an explosion hazard.
What do you do about the expiration containing vaporized virus? Wasn’t that what caused the spread ov COVID-19 at the nursing home in Kirkland, Was?
Not necessary. The Resmed 30 has an oxygen port that can be connected to the hose to deliver oxygen from a tank
Here’s an anesthetist explaining how to do it with standard hospital oxygen, some tubing, a bag, and a piece of a standard ER ambu bag. https://twitter.com/GellandMD/
Someone has modified full facial scuba mask and converted them to be a ventilator assist, not full invasive but positive pressure non invasive just like a CPAP.
With millions of CPAP machines it can’t be that hard to provide the positive and negative pressure and then add some type of HIPAA filter.
SOMEONE PLS TELL THAT VENTILATOR GUY THAT HIS 45CM-H2O PRESSURE IS TOO HIGH, IT WILL PUT SURROUNDING PRESSURE VIA THE LUNGS INFLATING, ON THE LOW PRESSURE ENVIRONMENT OF THE RIGHT-ATRIUM, THEREBY LOWERING BLOOD PRESSURE DANGEROUSLY, OMG -_-“
There must be millions of unused CPAP machines sitting on shelves in people’s homes. Does anyone know if the manufacturers are collecting machines and converting them. If this is possible, it seems like this would greatly reduce the time needed to get a lot of equipment out to those who need them.
I was thinking of the same thing, but using a BiPap machine, and a portable o2 generator. Just pipe the o2in at the mask. Doing a firmware update and software update on the unit to modify its function, I’m sure this could be done. I know my unit can be monitored through Wifi or cellular. Adapt a real ventilator hose to it , so you can capture the exhaled gases. All of this as a stop gap measure to fill a void where patients need some vent but are not at the point where they need a real ventilator. When they do, switch them over.
I asked the VA the same question a few weeks ago concerning the use of CPAP in cases not requiring full blown ventilators and they said they were already looking at doing so as an option. I wonder why this hasn’t gone mainstream. I even sent the question to news outlets to see if I could get anyone to ask that on the air or one of their endless medical experts. I just don’t understand why everyone is hyped up about plywood boxes and hand bags using motors to pump air when this is already available.
Air conditioner manufacturers would be very helpful in this area of expertise.
Just a word of caution about that article; it doesn’t give us any of the critical details about the story, like the name of the company that’s supposedly threatening legal action. The whole thing seems a bit too fishy, as there would seem to be a lot of red meat to dog into in a story like this and they just didnt. It wouldn’t be the first time that a Vox media story was found to be distorted, their business model is basically rage bait.
Apparently it´s a company in Luxembourg.
That narrows it down….
Vox Media narrowed it down:
Update, March 18th 5:30PM ET: A group of Italian volunteers distributed 3D-printed versions of a vital medical device — but it doesn’t appear that the original manufacturer threatened a legal crackdown.
(the company had simply refused to release design files and had not threatened to sue.)
I have a CPAP machine, actually two. They have electronic pressure adjustment and it would be a trivial task to modulate that pressure. No big deal. Such a conversion would not have all the bells and whistles of a $10,000 machine but it could possibly save a life.
Beyond that, I have used blowers in an aerospace environment. I could make design and build a workable ventilator in a day or two. Again, no bells and whistles but something to save a life.
ok were you here just to gloat on how trivial and no big deal it is or could you elaborate on that? hypothetically of course. That way there could be more of us out here able to do enough to save a life or several?
I have been thinking abut just that for a few days, it does not seem like much of a leap…..i was not sure how the pressure on the two compare.
Possibly so way to step up the motor on the CPAP to match the pressure on the ventilators…
Are there actually easy acessible specs as to what a device has to fullfill to work for (corona-case) ventilation?
E.g.
air-flow rates
air-pressure controllable between a..b
humidity
temperature
exhaling to somewhere else?
(let’s say apart from all that usual medical certification stuff)
A down and dirty chart… Not to be used for an end all beat all vent parameter list. But to answer your question:
https://www.rwhs.org/sites/default/files/airlink-factsheet-ventsettings.pdf
Thanks!
[ 5 cmH2O, now that seems to be some freedom pressure unit ;) ]
it’s a mechanical engineer’s unit, not a scientist’s unit
How many inches is that?
(Asking for an American friend.)
1 in water = 0.036 psi = 0.00246 atm
See Wikipedia, conversion of units. There, every unit of pressure is converted to pascal, Pa.
Each is shown to many more decimal places than are ordinarily needed. Also, numbers greater than 999 are shown in scientific notation. For example, a 10 followed by a superscript 3 means multiply the preceding number by 1000, since 1000 has three zeroes.
So the conversion is (1 in water = 249.1 Pa) / (1 psi = 6895 Pa) = 0.036 psi per 1 in water.
Thank you Thomas!
WHO had published a list of equipment needed to treat COVID19 patients. IIRC it included flow rates etc…
Please be cautious
it is not about cobbling together a device that behaves exactly like a medical ventilator for 5 minutes, including all measurements.
You have to build a device where the smallest malfunction could risk someones life or burn down the hospital.
You and the MD’s have to trust this device to work flawless for days, weeks, months unsupervised, connected to the hospital UPS powergrid, running on 100% oxygen, keeping someone alive, not bursting up in flames, not leaking oxygen, not rupturing someons lung or suffocating them. Still not included all forms of suboptimal ventilation that will not suffocate the patient or rupture his lungs but worsen the recovery or completely hindering recovery.
Please do not dissasemble working medical equipment, it could help someone else when supplys run short.
Regarding the italien 3D-Printed valves:
They are not tested, doctors know this, therefore devices fitted with this spare part will be very closely monitored, binding valuable personnel.
AFAIK: These valves are oxygen enrichment valves, they will be monitored like a handgrenade without a pin, as a small leak could lead to an O2 rich (combusible) atmosphere in the vicinity of this device. O2 leaks have always been an explosion hazard in hospitals, that’s why there are O2 shutoff valves on each corridor, that’s what caused the chinese hospital to blow up.
There’s so much fear-mongering about medical devices. If your options are certain death from pneumonia or possible death if the hacked-together ventilator craps out WHILE YOU’RE IN A HOSPITAL AND BEING MONITORED CONTINUOUSLY, I know what I’d take.
Not so sure about that: given the high pressures needed to ventilate these sick lungs and the risks involved doing that with even the most state-of-the-art ventilators, mortality rates would skyrocket…… (I’ve worked with a lot of ARDS patients in one of the best ICUs in Western-Europe at the time, it is never easy to ventilate very sick patients even with a modern ventilation approach, let alone with cobbled together equipment. McGyver has no place in a serious ICU)
given a 100% chance of death without intervention, and a 50% chance with an field-expedient solution, I’ll take the field-expedient solution
Ok Albert, you dont get one. Sign this waiver.
No you don’t.
First off even if the ventilator is availabl;e you need a ICU to intubate and respiratory techs to administer the machine. Both of whcih are in very limited supply. It is also very costly to put a person in a ICU.
Secondly, most people if they are elderly or if their cardio-pulmonary system is shot and are put on a ventilator will die anyway. As it is a last ditch option to keep that person alive.
In people with pneumonia whose lungs are filled with fluid you do a Broncoscopy to get rid of the fluid you do not intubate.
I’ve worked in medical device development in the respiratory field. I have not specifically developed ventilators, but I have met lots of respiratory techs. Let’s just say that in a pinch, I am sure other medical professionals could handle the very specific tasks of monitoring people under ventilation. Furthermore, my point is that if you have 10 people that stand a good chance of dying anyway and you have only 5 ventilators, wouldn’t it be nice to have some more options?
Well said Captain.
The way I see it is, it’s like the situation where you’re on a river bank and seeing someone drowning, you have available an empty gallon jug and 50ft of paracord, do you listen to the idiot who’s spouting off about it not being a coastguard approved lifesaving device, the paracord not being rated for live loads, etc etc, or do you just tie the cord to the handle quick and chuck it to them.
per and ER doctor: 10 inches of water on inhale, 5″ of water on exhale. the exhale needs to be filtered with .3 micron pore size
DIY BLDC centrifugal blower modeled on a CPAP blower: https://drmrehorst.blogspot.com/2018/04/the-mother-of-all-print-cooling-fans.html
CPAP?
I misread that first P as an R, and had a very different expectation for this article…
I was having the same problem with some other acronyms being used recently.
Look! squirrel. I wish WordPress was consistent between the app and the web version. I can “star”/like in the app but not here. If I read a comment in the gmail “browser” I can do something else. I guess if it was really a problem I would have a more definitive description of the issue.
All that to say, “like”
the proverbial SHTF? :D
Haven’t read the article yet, but wanted to ask a new question:
Is there a way to DIY Oxygen?
Hydrolysis of water should seperate oxygen and hydrogen.
That takes a lot of energy. It should be possible to make a DIY oxygen concentrator that does the job with far less energy. Check out wikipedia for a starting point.
Oxygen filters (and compressors) are rented for home use, if your are wealthy and have a doctor friend to prescribed. Actually, the filter passes N2 and only O2 remains. I’ll bet that one of these O2 units can’t supply a high enough rate to cause O2 toxicity, an inherently complete safety feature.
Your typical oxygen concentrator produces 5 liters a minute. I have a pair of them for mad science. I suspect the sieves are not in perfect shape and the oxygen is less than perfectly pure but for the mad science I use them for they work great.
pressure swing asorbtion concentrators are just 2 (or more) pressure vessels filled with suitable adsorbtion media, several valves with some control system, a lot of tubing and a compressor (with a filter)…
hydrogen peroxide catalyzed by manganese dioxide
Electrolysis of water works, but you have to get rid of the hydrogen. Otherwise BOOM! An oxygen concentrator would be better and safer as it would provide air enriched with O2, not pure 02, which is very dangerous also.
absolutely / industrial / welding tank oxygen is available in great supply , just not ” certified” but filled from same source as the medical oxeye tanks at the vendor . Divers use it in a pinch regularly !!!
Divers use compressed air not oxygen. Pure oxygen would KILL the diver. That is why
deep sea divers use a Nitrogen/Oxygen mixture.
Especially if that $11000 price tag for that plastic valve is real. That already makes me want to call them a certain male body part however if they sue the creators for 3Dprinting that valve in these times with that many COVID-19 cases like in Italy, it really makes me wonder whats going on in there heads.
That price tag seems a bit rich it’s only about AUD$25K for a compete machine. But they don’t specify WHAT machine the have built the part for
You just destroyed a properly working medical device -just why??? The CPAP fan could have saved someones Life by assisting the persons breathing untill a ventilator is available or maybe the support of the CPAP could be enough for the patient to recover. Not everyone needs to be intubated.
No sane physican would use the thing you build, it is dangerous because you eliminated the safety parts that would have protected the patients loung of getting in too much air volume or pressure etc what causes severe damage.
If you have working devices which support breathing do NOT modyfy them, they could get purified by medical staff and used but just if they are still the way the manufacturer built them.
Know what your taking about before you accuse someone.
#1) The device may already have been broken. Bad LCD, Bad internal power supply or motherboard etc…
#2) There is no way CPAP is going to save someone’s life, its not a ventilator.
#3) There are no safety parts. That pump will in NO WAY shape or form be able to over force your lungs. It’s not like sticking a air compressor hose in your mouth.
On top of this, the device is his. He owns it. If he wanted to use it to blow up balloons with it, that is his choice.
Stop being over paranoid about this situation. It NOT like you catch it and die.
Actually, it doesn’t take much pressure to tear lung tissue, and sick lung tissue may be weaker than healthy lung tissue. A CPAP blower is capable of producing that much pressure. That’s why CPAP machines are regulated medical devices that have to be set up for the user by qualified/trained people and are not available off the shelf at Walmart.
CPAP machines do save lives, but not directly. By allowing people to get proper sleep, they prevent a lot of car and industrial accidents that would be caused by people falling asleep at inappropriate times.
Not exactly, the sleep clinics basically put you on a machine that uses all the different pressures to see what is the one your apnea best responds to. Yes this done in a controlled manner, but if they were capable of rupturing lung tissue, I don’t think they’d do the “try all the pressures!” approach. Maybe you don’t get referred if they think your lungs are super delicate though.
Hmmm. It seems more likely they’d start at a low pressure setting and then slowly ramp it up until it solves the problem (keeps the soft tissue from closing the airway), at which point they’d stop increasing the pressure.
Actually there are auto-CPAP machines that deliver pressure within a set range. Doctors determine the range based on the severity and frequency of apnea episodes seen in an initial sleep study. Following this trial time, a proper pressure is determined and set going forward.
something related to check out, although not open at the moment:
http://www.freepatentsonline.com/20190336713.pdf
the Umbulizer, an automated bag type ventilator at about a quarter the cost of a regular ventilation machine.
The umbulizer is applying for a patent. Please could someone explain what aspect they are attempting to cover with the patent protection? Seems like there is prior art to at least the band method of compression (although it was not preferable to the cam method in the paper) https://web.mit.edu/2.75/projects/DMD_2010_Al_Husseini.pdf
I found that link on the openlung repo readme.md https://gitlab.com/TrevorSmale/OSV-OpenLung
And I’m concerned that umbilizer would take legal action to deter the openlung attempt to help the current emergency.
The big issue is filtering the air that comes out of your device. NIV can’t be used because it sprays the infected air from the patients lungs into the surrounding air. Infecting everyone in the vicinity.
portable greenhouse, vacuum cleaner, window…. or other such expedient measures should be higher priority/better than things not certified to be in contact with a patient, nobody seems to be taking to that idea or other nebulisation reduction strategies. Maybe it’s already calculated in as buffer while they get the politicos moving on coughing up more to accelerate the ideal equipment.
And yes for the comprehension impaired, we know proper certified medical equipment is better, nobody is saying chuck that out, here comes the saviour hackers with a 3D printed miracle machine, when there is none left unused, that’s where pragmatism should take over, next best, next best, next best, next best until you’ve got desperate relatives taking shifts with the manual ventilator.
Send it through an electric arc before discharging it outside. The intense UV and ozone generated by the arc will rapidly destroy any bacteria and viruses in the air.
just a thought ,I work in the HVAC field / there are readily available (small) germicidal UV lights everywhere , they are designed to be installed in a residential furnace
Useful tips! I did have a look and modified pressure sensors could feasibly be used. I made a setup using a BMP085 and needle as an interface a while back but haven’t used it in a while. (disclaimer: BSc MEL so I know a few things)
Given the shortage of hospital rooms alternative locations to provide treatment are required. Devices that allow for Remote Patient Monitoring (RPM) (e.g. pulse oximeters, medication dispensers) would allow, low-risk, infected individuals to remain home, allowing vital hospital beds to be available for the most severe cases. Advances in RPM devices, to monitor dehydration and in-home ventilation would further enhance home-based care, supplemented with appropriately trained home care support (e.g. nurses, home health aides, EMTs). It is encouraging to see this group working on such a noble and needed approach to this crisis.
We’re waiting for him to demonstrate its effectiveness by spending a couple weeks walking around a hospital with no PPE while administering blessings (or whatever) to seriously ill covid-19 patients. The patients will be the control group, getting real medicine. He’ll be the treatment group, getting whatever he thinks will work.
Great idea. Let’s home all of the televangelists pitch in to help this way!
A little off topic, but since we’ve already gone there and everyone’s irony meter needs a workout after being stuck at home all week…
News from California (natch) where a Covid-19 has delayed the planned opening of a major new facility dedicated to faith healing.
https://www.charismanews.com/us/80349-morris-cerullo-s-worldwide-legacy-event-postponed-due-to-covid-19-pandemic
My apologies if anyone was hurt by their irony meter exploding just then, but you *were* warned.
(Also, though the grand opening of the center itself will be postponed indefinitely, the on-site steakhouse restaurant *is* still open, if you’re feeling a bit peckish.)
Sorry, that was a reply to Reg’s comment about Jim Baker, above. for some reason my comments are not attaching in the right place
I saw the comment and do find it very humorous. Right up there with the people mobbing the store that just got a fresh shipment of face masks – right off the boat from China.
This particular project was posted to our facebook group of doctors and med tech R&Ds and deleted by the moderators there. It is a waste of equipment, and reduces the effectiveness and controllability of a perfectly good CPAP machine already designed for this task.
I wish I had access to the peer review notes before they were deleted, I would post them here. Let me see if I can request them and get them submitted to the HAD team.
I am very surprised to see it here this morning.
What’s surprising is how incapable people are of considering the possibility that with enough constructive input, this sort of ingenuity can become a viable solution that’s a net benefit in our common effort to overcome a dire situation.
If you believe everything should be a perfectly functioning success and up-to-standards on the first iteration, what are you doing here on hack-a-day? Otherwise, if you understand that this community has an extremely great amount of brainpower and the resourcefulness to incrementally improve projects to an acceptable level of quality and necessary functionality, what exactly surprises you?
You can get access to clinician’s controls for most APAPs. You can set starting pressure up to 20 cm H2O For starters, I intend to hack in a variable timed 1 cycle switch, and use manual cycle trigger to learn what settings work (or not) for me. A guy calling himself “the lanky lefty” publishes the way to get the hidden menu for a few different machines. Good breath to you who might want a breath of fresh air (humidified if you wish)
Yes, not a problem.. I just posted a response on a similar comment, Lets do it folks
Hey if the government wants to build a ventilator all it takes is a General and a small group of soldiers. In times of National Emergency the government will do what they want to do. There is no need to reinvent the ventilators. Just build the damn things.
-1 karma for not validating shit you write in a public forum.
> Just to confirm that recent reports from Italy are totally incorrect, we were contacted at the end of last week for manufacturing details of a valve accessory but could not supply these due to medical manufacturing regulations, we have categorically not threatened to sue anyone involved. The valve is an accessory supplied as part of a CPAP Hood system which alone costs a few euros.
The article has been updated – the guys deny they have been threathened, and the manufacturer also states they have not sued anyone.
That assertion has been disproven. https://www.theverge.com/2020/3/17/21184308/coronavirus-italy-medical-3d-print-valves-treatments?fbclid=IwAR0tcwQWJmkVutGPqUowSHCtC1jlc15Y4I96Y1-MNe7CvBsI8ZgS1FN5Xb0
I don’t know if it’s been posted yet, but this family managed to keep their son alive for 7 years after he was paralyzed from the neck down by using a very simple diy ventilator:
https://www.dailymail.co.uk/health/article-2270178/Chinese-man-kept-alive-years-HOMEMADE-ventilator-family-squeeze-18-times-minute.html
Could something like this be used for Covid-19 patients? The circumstances would be much different, given that the paralyzed man presumably had normal lung function, but a similar device still might fulfill a niche.
I’ve got a TAZ 6. Also have a spare Windows 10 machine to add to a cluster. How can I help?
@john bates
https://gitlab.com/TrevorSmale/OSV-OpenLung
https://opensourceventilator.ie/
https://panvent.blogspot.com/?m=1
https://agentgallery.com/objects/rare-1965-prototype-harry-diamond-labs-respirator
https://www.helpfulengineering.org/
I wish some tech-oriented organisation with editing and content curation capabilities, as well as an online presence synonymous with not-exclusively-infosec hacking, would perform a public service and publish a moderated focus Web page for people wishing to help with technical contributions to the effort. Wink wink hackaday.
This is a great idea – adjustable CPAP needs to be paired with a helmet. This is all that is needed (other than optiflow), since intubation and ventilation has a mortality rate of 87% and ECMO mortality is 100%. So ventilators won’t save many lives (most people die anyways). But CPAP with helmet will save many more lives. The government won’t do any of this due to legal liabilities. People need to do this themselves – grassroots. This is a CHRONIC illness lasting weeks to over a month. Each critically ill person will tie up an oxygen delivery system for weeks. People keep shedding this virus for up to 37 days and are still actively infectious! Mortality in Italy is over 8% and will be higher in US due to governmental incompetence.
I believe you should say Bureaucratic incompetence, not Governmental incompetence. The bureaucrats won’t do any of this due to legal liabilities…. Lets at least put the blame where it truly belongs, with the pass the buck bureaucrats. Now, lets get back to if it will work, or could be simply modified to work until the proper equipment is made and available, then this temporary field triage could be a workable solution temporarily.
The question is not, “can a CPAP machine be a respirator.” Instead the question is, “Can a CPAP machine be better than nothing when a respirator isn’t available?” I say the answer is yes. In addition I have a SoClean unit that sterilizes it every day with activated oxygen. Adding oxygen to the air stream would be as simple as attaching an oxygen hose instead of the activated oxygen hose to the tubing adapter injector valve (see picture: https://www.directhomemedical.com/cart/merchant.mvc?Screen=PROD&Product_Code=dreamstation-systemone-hose-adapter-soclean-2-cpap&Store_Code=DHM&gclid=Cj0KCQjw9tbzBRDVARIsAMBplx9niczRuW1DJ0e-Q3f6pU3u0Q_VVSZ7sbXr893cqZt5N7PbITtoR8IaAowDEALw_wcB)
I have a bad flu which may very well be COVID-19 (haven’t been tested yet). Breathing was difficult when lying down and trying to sleep. However a combination of a CPAP, using pillows to elevate myself so I’m not lying flat, use of a Neil nasal irrigator 2-3 times per night plus lots of “farmers” nose blowing and deep coughing has gotten the mucus out and allowed me to sleep for 3-4 hour stretches. The CPAP is definitely helping.
I have a CPAP, and a so Clean, there awesome, and I also own an Oxygen Generator that can produce adustable up to 93%oxygen that can be adapted to a CPAP machine DEDAKJ Oxygen Generator DDT-1A-6L Machine bought thru eBay and are still available now.
I still have my previous CPAP and a new never used hose that I’d be happy to donate. Please let me know if anyone could use the CPAP or use it for parts. Thanks. Dianna
Is that still available? Can I buy it off you? My mom is old and getting sick. I’m worried she’s developing it.
This is why I’m here. Many of my older friends had CPAPS prescribed and couldn’t bear to use them there are thousands sitting in closets. I know we would all be thrilled to donate these units to fill the need to save lives. Less critical levels of ARDS could take pressure of demand for ventilators.
Thanks for all of this info. If a cpap is used for covid, should the humidifyer be used or will that increase chances of Pneumonia?
i dont believe from all ive read that it would increases chances of getting corona since Corona virus is gotten thru contact with other infected people and then touching your face, but it will stop dry mouth, But if you do have it it might decrease the rate in which you recover, In my educated opinion
Hi guys, could a full face snorkel mask be used? For docs and nurses, like you say its better than nothing? Some patients could use it with an O2 feed to help some patients. Can we just put an AMBU mask with a boxed in bag? Depressed by a piston type thing to squeeze and release the bag? A dc motor to control the speed and an air valve/O2 line to regulate flow?
Apparently there is a project that has been trying to consolidate the performance data from a variety of CPAP’s into a usable data set – could be a starting point for management. https://sourceforge.net/projects/sleepyhead/
If an unmodified and properly working CPAP is used, and 100% O2 is a concern, could one just use a nasal Cannula connected to an O2 tank to bleed some O2 into the nostrils, and then place the CPAP mask over it? The nasal O2 input along with the CPAP mask would deliver a mixture of normal air and O2. KISS solution?
I have sleep apnea and have used a BiPAP for 20+ years. This past year I’ve had to be on oxygen as well. I have an oxygen concentrator that is attached to my BiPAP/CPAP tubing. No need to use a canula when wearing the mask.
https://www.cpap.com/productpage/oxygen-enrichment-adapter
In January I was testing a non-invasive ventilator, but at the time I did not benefit from one. Plus that cost was $2000/month with having insurance. I’m in Ohio and work from home so I’m doing what I can to avoid COVID-19 exposure.
Engineering students may have answers:
http://m.facebook.com/story.php?story_fbid=10216948634770056&id=1291609238?sfnsn=mo
I have taken a ResMed ‘Escape’ model CPAP with heated humidifier. I tapped into the side of the humidifier tank and added a port for an O2 connection. I have connected a flexible hose from the mixing control/handle of my oxy/acetylene welder to the humidifier tank port I created. The pressure on the ResMed can easily be adjust with instructions available in the public domain. Welding O2 is not medical grade but neither is the air we take into our lungs each day. The ResMed is connected to a full face mask. I have not used it but if I reach a crisis stage and the hospitals are overwhelmed, I am hoping this will be a life saver combined with the practice of laying on my stomach, not my back.
My wife uses a Bi-Pap. Through a friend we contacted a doctor at John Hopkins about the use of a Bi-Pap as a ventilator. The response from this doctor was that the problem was that the Bi-Pap does not provide a closed system and you would spew virus into the surrounding environment. From my readings the Bi-Pap is the candidate for conversion to a ventilator in a hospital environment. The manufacturers are the only ones who can properly address this, everything else is dangerous.
I have a question, i have a NIV resmed cpap mask used before to only treat sleep apnea. If its just adding from any kind or source of oxygen, would that be the same as a ventilator at a hospital? i read that the recommended rate was 5l/m of oxygen for initial treatment for COVID by WHO, but CPAP’s air pressure is only positive air pressure correct? And that that would be intrusive for a inflammed lung? Then what does a ventilator do? and if its better than nothing, as i am living alone, if i had covid, would adding oxygen into the the cpap mask help at all and at what rate? Just trying to learn as i do not know any knowledge of anything and just thought of this today. Thanks in Advance.
Can’t developers make a CPAP or BIPAP into a closed circuit system?
I read something about Dr. Chistsi’s bubble CPAP. Putting the exhale pipe into water, that keeps the lungs open even during exhalation. So 75% death rate reduction. And one can maybe heat the water or make it full of detergents to kill the viruses.
CPAP can aerolize the virus and infect everyone in close proximity ti the particles
If you had the virus would you not be coughing and spewing contamination in the room regardless whether you had a CPAP or not?
https://www.oxygenconcentratorstore.com/blog/oxygen-user-question-what-oxygen-concentrator-can-i-use-with-a-cpap-machine/
Action Plan to Solve Ventilator Shortage
Upgrade CPAPs to Bi-PAPs and then to Non-Invasive Ventilators
The hardware used by home CPAP machines to treat Sleep Apnea can provide the essential functions of a Hospital Ventilator. CPAPs requires hardware modifications and replacement of software to become Bi-PAPs. With proper settings, Bi-PAPs can be Non-Invasive Ventilators.
There are millions of CPAP machines in the USA… 20% to 30% are not being used. We could collect them, upgrade the hardware & software, and then deploy them in hospitals in a week. Using 100,000s of existing CPAPs will cut the time to get Ventilators into hospitals from weeks or months to days.
How can we do this? Understand the Process. Find an alternate process using creative resources.
1. Have companies like ResMed and Philips Respironics stop making new CPAPs or Bi-PAPs and 24/7 produce CPAP MODIFICATION KITS to upgrade CPAPs to Bi-PAPs.
2. Have these companies also distribute Bi-PAP software that lets the Bi-PAP use ALL the capabilities of the units.
3. Have people donate EXISTING CPAPS to their local hospitals.
OR
1. Have hackers reverse engineer the hardware modifications and 3D print CPAP MODIFICATION KITS.
2. Have software hackers crack the software on the Bi-PAPs and distribute Bi-PAP software.
3. Have people donate EXISTING CPAPS.
OR
1. Use the War Powers Production Act to facilitate either or both above.
I have a Bi-PAP that is a CPAP with more advanced software and some internal “extra parts”. It monitors my breathing and provides 15 millibar pressure while I breath in and little pressure while I breath out. If I do not breath in soon as expected, the Bi-PAP provides up to 25 millibar pressure to get me breathing. It can be unlocked to deliver 40+ millibar. I am very unlikely to die without my Bi-PAP. I start breathing again naturally with a startle response that reduces the quality of my sleep.
COVID 19 patients going into respiratory distress, without mechanical assistance, will die.
Where can I donate my Bi-PAP? My getting poor sleep and being drowsy while awake is a trivial price for saving 1 if not a dozen lives.
Currently, the process alternatives are:
A. Build Ventilators. They are expensive and complex. To hard to be done in time.
B. Build Bi-PAPs. Cheaper and easier than Ventilators. Less efficient than C.
C. Manufacturers that are building Bi-PAPs can easily transition to CPAP MODIFICATION KITS and when married with existing CPAPs get 10, 20 or 50 times the units into hospitals.
I see reacting to the ventilator shortage as a process challenge. In a crisis, standard processes might not be up to the challenge. In this case, using alternate resources in a novel way (repurposed CPAPs) the time to solution can be greatly shortened. There are likely additional challenges to be identified and resolved. The process proposed above has overcomes some of the major challenges in traditional responses to this challenge. Box? What box?
Doug Jones, Partner
Process Renovation Consulting, Inc.
Champaign, Illinois
Action Plan to Solve Ventilator Shortage…. Upgrade CPAPs to Bi-PAPs and then to Non-Invasive Ventilators
The hardware used by home CPAP machines to treat Sleep Apnea can provide the essential functions of a Hospital Ventilator. CPAPs requires hardware modifications and replacement of software to become Bi-PAPs. With proper settings, Bi-PAPs can be Non-Invasive Ventilators.
There are millions of CPAP machines in the USA… 20% to 30% are not being used. We could collect them, upgrade the hardware & software, and then deploy them in hospitals in a week. Using 100,000s of existing CPAPs will cut the time to get Ventilators into hospitals from weeks or months to days.
How can we do this? Understand the Process. Find an alternate process using creative resources.
1. Have companies like ResMed and Philips Respironics stop making new CPAPs or Bi-PAPs and 24/7 produce CPAP MODIFICATION KITS to upgrade CPAPs to Bi-PAPs.
2. Have these companies also distribute Bi-PAP software that lets the Bi-PAP use ALL the capabilities of the units.
3. Have people donate EXISTING CPAPS to their local hospitals.
OR
1. Have hackers reverse engineer the hardware modifications and 3D print CPAP MODIFICATION KITS.
2. Have software hackers crack the software on the Bi-PAPs and distribute Bi-PAP software.
3. Have people donate EXISTING CPAPS.
OR
1. Use the War Powers Production Act to facilitate either or both above.
I have a Bi-PAP that is a CPAP with more advanced software and some internal “extra parts”. It monitors my breathing and provides 15 millibar pressure while I breath in and little pressure while I breath out. If I do not breath in soon as expected, the Bi-PAP provides up to 25 millibar pressure to get me breathing. It can be unlocked to deliver 40+ millibar. I am very unlikely to die without my Bi-PAP. I start breathing again naturally with a startle response that reduces the quality of my sleep.
COVID 19 patients going into respiratory distress, without mechanical assistance, will die.
Where can I donate my Bi-PAP? My getting poor sleep and being drowsy while awake is a trivial price for saving 1 if not a dozen lives.
Currently, the process alternatives are:
A. Build Ventilators. They are expensive and complex. To hard to be done in time.
B. Build Bi-PAPs. Cheaper and easier than Ventilators. Less efficient than C.
C. Manufacturers that are building Bi-PAPs can easily transition to CPAP MODIFICATION KITS and when married with existing CPAPs get 10, 20 or 50 times the units into hospitals.
I see reacting to the ventilator shortage as a process challenge. In a crisis, standard processes might not be up to the challenge. In this case, using alternate resources in a novel way (repurposed CPAPs) the time to solution can be greatly shortened. There are likely additional challenges to be identified and resolved. The process proposed above has overcomes some of the major challenges in traditional responses to this challenge.
Doug Jones, Partner
Process Renovation Consulting, Inc.
Champaign, Illinois
I did not have time to read this this wall, but I wanted to add a suggestion. I have been thinking about a modification kit also. If a Ventilator just delivers are and the lung naturally exhales while on a vent then maybe the CPAP is the answer. Can we split the CPAP line with a “Y” , put a solenoid driven valve on each side of the top of the “Y”. One valve is naturally open and the other is naturally closed. Then take an infinite loop timer ( https://www.alibaba.com/product-detail/CN102A-small-microcomputer-circulation-control-switch_60820722451.html?spm=a2700.galleryofferlist.0.0.13bc12c2fbl0Mz ) hooked to each solenoid. the bottom side of the “Y” goes into the intubation tube, one side of the “Y” goes to the CPAP and the other is the exhale tube. You can also add a nipple upstream for Oxygen. best of luck to all of you.
Cpap ozone sanitizers use hose adapters that could be used to supply regular O2.
It seems to me there could be one BIG air oxen supply that could serve several patients, Each patient has a computer controlled valve, it is done all the time in the auto world fuel injectors they open and close depending on the readings from vacuum sensors air flow sensors and O2 sensors. It would be kind of a daisy chain supply but each patient would only use part of the supply. We are talking about a lot of people needing breathing help at the same location. it would seem like les parts to build.
some thing to discuss is what to do with the exhaled air to avoid spread of disease we need to hook it up to a electronic air cleaner to avoid contamination of surrounding area
Could the calibrated exhaust port on the mask have a hose adapter added and a hose connected to the uv cpap cleaner to kill any virus being exhausted . This might protect others.
read Dr. Chistis bubble CPAP. exhalation goes into water. Maybe we can fill the water with detergents to kill the virus.
Auburn Engineering School converts Cpaps to Ventilators
http://ocm.auburn.edu/newsroom/news_articles/2020/04/020930-cpap-machines-ventilators.php
Holy Crap- Where have I seen this outstanding idea before:
29 March 2020
“I did not have time to read this this wall, but I wanted to add a suggestion. I have been thinking about a modification kit also. If a Ventilator just delivers are and the lung naturally exhales while on a vent then maybe the CPAP is the answer. Can we split the CPAP line with a “Y” , put a solenoid driven valve on each side of the top of the “Y”. One valve is naturally open and the other is naturally closed. Then take an infinite loop timer ( https://www.alibaba.com/product-detail/CN102A-small-microcomputer-circulation-control-switch_60820722451.html?spm=a2700.galleryofferlist.0.0.13bc12c2fbl0Mz ) hooked to each solenoid. the bottom side of the “Y” goes into the intubation tube, one side of the “Y” goes to the CPAP and the other is the exhale tube. best of luck to all of you.”
Please excuse my ignorance. If an APAP machine detects inhale and exhale, then why isn’t that enough to ventilate a patient. And yes, I’m asking specifically about someone who is infected with Coronavirus/COVID19 and is having trouble breathing. I used to have an APAP machine from Fisher & Paykel and it detected all this stuff automatically. Especially if you’re saying that there are APAP machines with a tube for O2, and you can buy O2 generators on Amazon that sync with the APAP machine, then isn’t that a slam dunk? I’m not talking about someone who is in critical condition – just someone who is struggling to breathe and who’s O2 is down quite a bit.
FYI – I don’t have Corona, but the hospitals may soon run out of ventilators and I still have a script for a CPAP/APAP machine, and I’m just trying to plan for the future. Also, my parents are in their late 70’s, so it’s a huge worry. Thanks for your help!
For those wondering how high oxygen content and sparks react, read about Apollo 1. They died from the fire caused by a spark in an oxygen enriched environment. The USAF use to warn us about mustache wax and going to 100 % oxygen. There are some good ideas and dangerous ideas. Choose wisely
About CPAP’s contamination problem, I read something about Dr Chisti’s bubble CPAP. The exhalation goes into water (creating bubbles) and it provides a pressure to keep the lungs open during exhalation. 75% death rate reduction. Maybe one can fill the water with detergents to kill the virus when it enters the water.
Last year I used my ResMed machine for sleep apnea when I had the flu last year and I put it on and went to sleep I woke up I was short of breath so do use it if u don’t have nothing else but at least be active so u can breath on your on with just the right amount of assistance from the machine u have to have some strength to fight it it worked for me last year I needed air I got some