Designed to be used once and then disposed of, personal protective equipment (PPE) such as N95 face masks proved to be in such short supply during the early days of the COVID-19 pandemic that getting a few extra uses out of them by sanitizing them after a shift seemed smart. And so we saw a bunch of designs for sanitizing chambers, mostly based on UV-C light and mostly, sad to say, somewhat dodgy looking. This UV-C disinfection chamber, though, looks like a much better bet.
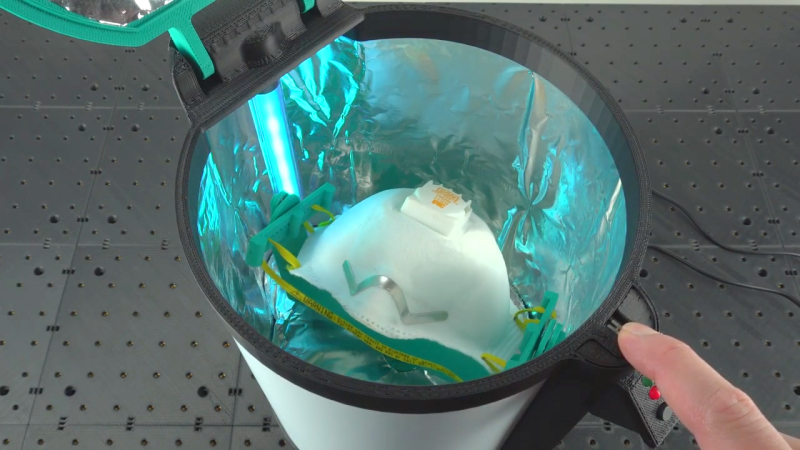
The link above is to the final installment of a nine-part series by [Jim] from Grass Roots Engineering. The final article has links to all the earlier posts, which go back [Jim]’s early research on UV-C sanitization methods back in March. This led him to settle on an aquarium sanitizer as his UV-C source. A second-hand ultraviolet meter allowed him to quantify the lamp’s output and plan how best to use it, which he did using virtual models of various styles of masks. Knowing that getting light on every surface of the mask is important, he designed a mechanism to move the mask around inside a reflective chamber. The finished chamber, which can be seen in the video below, is 3D-printed and looks like it means business, with an interlock for safety and a Trinket for control.
We love the level of detail [Jim] put into these posts and the thoughtful engineering approach he took toward this project. And we appreciate his careful testing, too — after all, it wouldn’t do to use a germicidal lamp that actually doesn’t emit UV-C.















A simpler solution is to keep the PPE in a warm and dry place for a few days.
Assuming you have enough to cycle through in the mean time.
True, but that also applies to the UVC method. Since you can only reuse them a limited number of times, both methods require a steady supply.
Or the dryer for 20 minutes.
Though that would use considerably more energy….
I thought about building rooms in hospitals or steel lorry containers 8 weeks ago but if it was viable someone would have already thought about it, I’ve just got my uv and ozone light sorry
Reasonably powerful bulb, good, exposure time, yeah, wishful thinking again. While he has actually used the right figures for coronavirus 1mJ/cm^2 instead of the feeble 10 times less power required to get rid of drinking water concerns like giardia and e-coli, it seems he has forgotten that he has a limited kill zone right next to the lamp, and while he calculates that half the mask is exposed at once, it’s obvious to the naked eye that no more than a quarter of each side is getting adequate exposure at any one time. Therefore it needs 4x longer exposure at least, if not 6x. Also the inside front of the mask cannot get nearer than about 3″ plus the clearance to the bulb, so that gets 16x less exposure than all the parts that can be rotated close to it. Since I would worry that the valve area could be a trouble spot, virus getting sucked in during the time it takes for the valve to close on inhale, so being on the inside of the valve there, then this is cause for concern.
Just did one of these, and had a really good team for it.
We ended up using ray tracing to map the direct and indirect paths for our 438W, with 146W of that being pure UVC, using a 60% bounce off polished AL. We needed 12 elements to get even coverage with acceptable drop-off.
End result was worst case kill time for direct exposure of 10s anywhere in the 27^3 in box.
but then in that case you are assuming that there is no light energy at all also being reflected all around the chamber during the entire process?
It’s falling off with the square of the distance so it’s 16, 25, 36, 49 etc times weaker for increasing path length so it is not going to reduce effective exposure time by more than a few percent.
It’s a tube nearly as long as the chamber, not a point source. 1/r^2 is not a valid approximation.
What is the appropriate equation for a tube source?
The intensity falling off as the square of the distance applies to point sources. When you have a line source, and am close enough to it that it is more like a line than a far-away point source, it falls off linearly. If the light source is a plane source, the intensity does not fall off with distance at all. His container with reflecting walls might be close to a plane source.
in one of the posts he actually 3d plots the energy output in the cad…
All good points. I didn’t see his calculations, but do you believe that he did not calculate his worst case / greatest distance? Very true about the exhalation valve in the demoed respirator.
I’m Co-Founder of UVENTIONS, a company that specializes in UV-C disinfection systems.
We’re currently also building a disinfection system for face masks that’s certified as lab equipment and will be available mid-july.
Getting these things right, i.e. an even radiation across the whole mask is pretty tricky because all the optics/shadows/reflections involved, but once you have it, they work great. The microbiology lab we work with was really surpised how well it worked..
Simple solution. Stick a stepper motor in the lid, with a string hanging from the shaft. Attach mask to string and slowly rotate the motor. Its not rocket science guys.
This seems like the right answer, rotisserie that thing!
But then you would end up with consistent shadows?
Has anyone considered using ozone to sanitize masks ? Like building a high voltage ozone generator ? Or how to hack a CPAC cleaner (SoClean?) to clean masks or incoming mail ? Although you might have to one run ozone generator in a box outdoors so you don’t get ozone filling the house.
Ozone is rather aggressive to a lot of materials. I have my doubts whether the filter material could stand up to it for long.
The UV-C lamps will produce a substantial amount of ozone as a byproduct. I am using a similar UV-C sterilizer box built from a pair of fish tank lamps and the ozone stink is very noticeable after a few minutes of use.
Ozone production is dependent on the wavelength of the UVC light produced. At less than 220 nm there is Ozone production. At 254 nm UVGI ozone is not produced. https://www.light-sources.com/solutions/germicidal-uvc-lamps/uv-germicidal-lamps/uvc-ozone/#:~:text=UV%20wavelengths%20harnessed%20at%20185,produce%20ozone%2C%20(O%C2%B3).
I believe the production of Ozone or not, is just down to the particular glass used. Both lamps are essentially Hg fluorescent bulbs, without the interior coating and using glass that passes the desired wavelengths. If you want ozone, you pass 220nm. If you don’t, you pass 254nm. Both are spectral lines for Hg. 254nm bulbs are 33% efficient. Those producing ozone are slightly higher.
All conjecture, but it makes sense to me…
Just as an FYI: The current OSHA permissible exposure limit (PEL) for ozone is 0.1 part of ozone per million parts of air averaged over an eight-hour workshift. But the NIOSH Ceiling limit is the same as the PEL. The IDLH is only 5 ppm. So be careful what you breathe if you can’t measure it. It would be sad to protect you lungs, etc from the virus and hurt your lungs with a lamp.
Others have used H2O2 (hydrogen peroxide) vapor to sanitize masks.
It’ll decomposite down to water vapor. Google for “h202 vapor mask santization”
I find it interesting that the efficiency of an N95 comes from the electrostatic charge placed on the mask during manufacture. One cannot wash the mask or use alcohol on them to clean them because it removes the charge which would then make the masks capture efficiency equal to the much larger pore size of the filter – “ineffective” against SARS-COV-2. (Forgetting cloth masks or coffee filters). Yet breathing though the mask introduces water vapor, and H2O2 breaks down to water. So how does use or H2O2 not accelerate the breakdown of the masks? When I asked at the AIHCE, a conference of Occupational Health Scientists a couple of weeks ago, the only thing anyone who would speak up would quote the NIH study… but they (NIH) were under significant pressure to provide guidance in these “unprecedented times.” When I asked if anyone had done a critical read of the NIH studies as I had, no one replied. From what I have seen, I have a very reduced confidence in the accuracy of the information from those tasked with coming out with recommendations. Those recommendations to which the public clings. And in these times an old N95 is likely still better than the surgical masks they send a majority of medical staff out to interface with their “Covid-questionable” patients and fellow staff.
How does the UV breakdown of the mask material affect micro-plastic inhalation levels?
How much of the viral/bactrial/fungal load in a facemask is on the visible surface, vs. inside the mask?
How well does UV disinfection work beyond the visible surface?
How much of a infection hazard are pathogens below the visible surface?
(i.e., does this just disinfect surface – so touching it is unlikely to spread pathogens,
vs. pathogens which might be released into air when breathing through the mask)
Still only a 3 log maybe 4 log reduction of pathogens, not to mention the polymers that breakdown because of exposure.
If you wear a mask for 8 hours, then 3 log reduction means it’s refreshed to same level as wearing a new mask for 29 seconds, which would be good enough.
When I set out to make a decontamination box myself, over a month ago, UV initially looked like a good candidate, but I did not choose UV sterilization because some papers mentioned degradation of the filter material and weakened straps. Besides that, figuring out how to deal with shadows and varying distances to the light source seemed pretty complicated. Some background information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4699414/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202248/
So I went with dry heat. Not too much heat, because that would obviously degrade the plastic filter material (which appears to basically always be polyproylene — do non-PP respirators or filters even exist?). After considering several ways of building this, it seemed that a cheap heated bed for a 3d printer (switched with a relay) and any polypropylene box such as an Ikea Samla, and a few DS18B20 temperature sensors to build a fast acting thermostat (want to keep the temperature above 70° C, but below 100 °C), would easily do the trick, maybe with some extra thermal insulation (nested Samla?).
That project would have been simple and cheap, but when googling for heat boxes I discovered a commercial kitchen appliance called a “warming drawer”, which is basically a heated bed in a box. That looked like a good shortcut, so I bought a used one online, put an Ikea Samla in it with a few DS18B20 temperature sensors hooked up to an ESP32 (on a borken SHA2017 badge), and several test runs showed that it reaches at least 70° and the hottest spot is around 80°. I decontaminate 3M 2135 and 2138 filters in it, not just face masks, by simply putting them in the small 5 liter Ikea Samla, putting the Samla into the warming drawer, and turning it on at its highest heat setting. It then takes about 15 minutes to heat up, after which I wait another 60 minutes (one study suggested 30 minutes should suffice, another said 60) just to be sure. I always keep a temperature log to make sure the box stays at the right temperature during the whole decontamination cycle.
A picture of an FFP2 (European N95 equivalent) respirator in a samla in a warming drawer, with temperature sensors: https://twitter.com/Whreq/status/1261359274891948033
Source of the very simple Arduino sketch that I use to broadcast the temperatures over MQTT: https://github.com/Juerd/thermo/
I’d be interested to see your project results. Please share more!
We went the UVC route as we needed to sanitize in seconds, but there will be consequences for this as you have noted.
I’d like to share more, but don’t know what else I could share. If you have any questions, though, just ask!
Yes, I’ve just been using a domestic oven for personal mask recycling needs, after reviewing all the possibilities. Mine can only be set as low as 170F which is ~76C at which temperature I have found no problems with premature mask ageing thus far. I only have about 4 cycles on any of the masks though. I preheat to set point temperature, put mask in on insulated baking tray (double bottom) wait 5 mins, verify with IR thermometer that 70C is reached, set timer for 30 mins… and I haven’t needed to use the oven for anything else right after, so I have been just turning the oven off and letting them cool down inside it, so they probably get another half hour of 50C, half hour of 30C and down near ambient again. They seem “fresh” after this treatment. In fact one small package that had been in a corner of the basement for some years and had a faintly musty odor improved with baking. These were “surgical/procedure” type masks, of cheap manufacture, not supplied as sterile.
I read the NIH studies a while ago, they are widely quoted however, they did not seem to have a good handle on how much light to use and if I remember correctly, used nearly 300 times the required level of UVC to kill SARS-Covid-2 and does not adequately describe the UVC test design. Yet denotes 3 uses of UVC ruins the masks. It seemed biased toward H2O2 chambers. Yet, i found other studies that were not quite so rushed on a UVC Association website, one by Florida based engineering firm that seemed particularly well designed and documented. The Florida engineering firm used many brands and ranked wear and longevity of the masks. It was significantly longer than the NIH studies indicated. Additionally, the NIH references appear to quote eachother and on old research mostly regarding bacteria. The Florida work has been continuing for 10 years. Additionally, how the user treats the masks has a lot to do with its longevity.
I believe this was the source of which I spoke above: https://www.ara.com/sites/default/files/MitigateShortageofRespiratoryProtectionDevices_2.pdf
Cycle = use/treatment
Stanford University Medicine – Addressing COVID-19 Face Mask Shortages [v1.3]
https://elautoclave.files.wordpress.com/2020/03/stanford-2020.pdf
In this materials science study of N95 face masks, two disinfection methods which do not reduce the filtration efficiency of the meltblown layer after an appreciable number of treatment cycles were found:
• Method 1: 75°C Hot Air (30 mins) for 20 cycles
• Method 2: UV (254 nm, 8W, 30 min) for 10 cycles
The issue I had with this study was with the “8W, 30min” for only 10 cycles. They did not discuss any distance measurements or if the 8W was of UVC or an 8W bulb that produced UVC. If I recall, no attempt was made to quantify the dose received by the respirator material as has been an issue for most studies of this type that I have encountered. Basically, we have a UVC bulb in a toaster oven and ran it 10 cycles. Why also not run more than just 10 cycles like to failure or some incredibly high number?
This is their “sterilizer.” Originally designed for nail care. http://www.berkeleybeauty.com/i/proddetail.php?prod=ST208A-US
All this care for their mask and complete disregard for people around them… Masks with VALVES allow free flow of air out, i.e., all your COVID goes out unfiltered. Not nice. Not nice.
These are used in a hospital situation where doctors are exposed to infectious patients. It would be inappropriate in public.
A person (not in the front line) wearing a N95 grade mask would have a lower chance of catching the virus in the first place.
Masks with valves are intended for industrial use to protect the wearer from airborne particulates. Medical N95 masks do not have the valves so they filter air in both directions.
https://www.fastcompany.com/90496717/what-is-a-mask-valve-and-why-are-cities-banning-them
If you want to wear an industrial N95 mask in public, then wear a cloth mask over it to protect people around you from your exhalations. The industrial N95 will protect you. The cloth mask will protect others equivalently to wearing a cloth mask alone.
I simply put a piece of tape over the valve on my masks, on the inside. Problem solved.
I suggest also placing a bit of tape on the outside then to avoid judgment of others.
Wrong, especially with professional masks like 3M. Masks with valves are designed differently compared with masks without valves. Exhaling into a valved mask with a blocked one-way exhaust valve loads up the blown plastic and other material layers with moisture. In most professional masks like 3M the mask material creates an electrostatic effect to capture particles better, moisture compromises this effect. the best thing to do is wear a surgical mask over a valved mask or better yet cut a square of surgical mask and tape it to the outside over the valve. Once you do that you don’t need the valve any more, so remove the one-way valve flap to reduce flow resistance. Cover the outside of the valve so people can see it, that may stop some Karens from barking at you in public for wearing a valved mask – but not all of them. Beware the Karens!
Thanks for pointing that out to the group.
This DIY home UV sterilizer is the best I’ve seen so far: https://www.sublimelight.art/Photo-Galleries/UV-Sterilizer/. Good UV uniformity, high power. Hope it helps
guys what about using the microwave oven
June 2004 issue of the Avian Pathology journal, where an Avian Coronavirus called IBV was killed after being microwaved for 5 seconds2.
https://www.tandfonline.com/doi/full/10.1080/0307945042000205874
This is fake science. Sure, the UVC kills germs but you can’t buy or build a UVC lamp system that fills all the shadows in any situation. All you can hope is to reduce the number of germs in an exposure so that your body has a better chance of fighting it off but you can never be sure. In an empty hospital room, combined with serious effort at wiping things mounted to walls, etc., you can reduce germs but you’re only saving some labor. The lights can only get the surface and the things you can easily see and reach to wipe. It can save a few hours work of a housekeeping worker and it might be more reliable on the surfaces the light reaches but still, and in the final equation, the light only kills germs where it reaches. Germs in the shadows begin to spread immediately when the light is off.