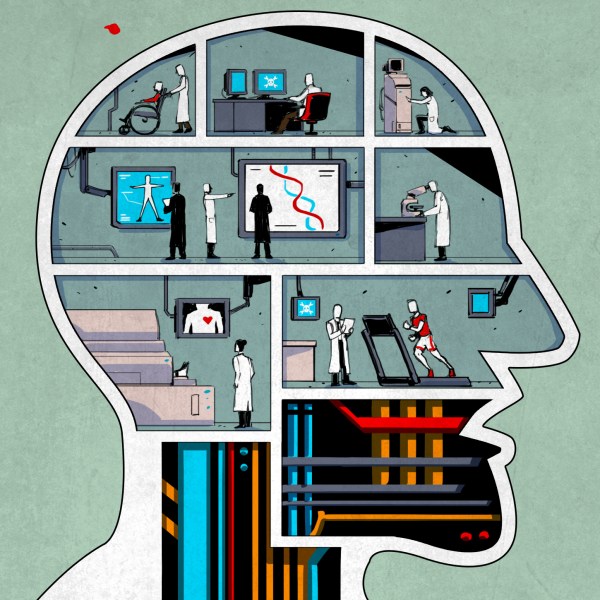
An interesting and also annoying aspect about the human immune system is that it is not a neat, centralized system where you input an antigen pattern in one spot and suddenly every T and B lymphocyte in the body knows how to target an intruder. Generally, immunity stays confined to specific areas, such as the vascular and lymph system, as well as the intestinal and mucosal (nasal) parts of the body.
The result of this is that specific types of vaccines have a different effect, as is demonstrated quite succinctly with the polio vaccines. The main difference between the oral polio vaccine (OPV) and inactivated vaccine (injected polio vaccine, or IPV) is that the former uses a weakened virus that induces strong immunity in the intestines, something that the latter does not. The effect of this is that while both protect the individual, it does not affect the fecal-oral infection route of the polio virus and thus the community spread.
The best outcome for a vaccine is when it both protects the individual, while also preventing further infections as part of so-called sterilizing immunity. This latter property is what makes the OPV vaccine so attractive, as it prevents community spread, while IPV is sufficient later on, as part of routine vaccinations. The decision to use a vaccine like the OPV versus the IPV is one of the ways doctors can tune a population’s protection against a disease.
This is where the current batch of commonly used SARS-CoV-2 vaccines are showing a major issue, as they do not provide significant immunity in the nasal passage’s mucosal tissues, even though this is where the virus initially infects a host, as well as where it replicates and infects others from. Here intranasal vaccines may achieve what OPV did for polio.
Continue reading “Intranasal Vaccines: A Potential Off-Ramp For Coronavirus Pandemics”