[Gui Cavalcanti], whose name you might recognize from MegaBots, got on a call with a medical professional in San Francisco and talked about respirators. The question being, can we design and deploy an open source version in time to help people?
Unnerving reports from Italy show that when the virus hits the susceptible population groups the device that becomes the decider between life and death is a ventilator. Unfortunately they are in short supply.
The problem gets tricky when it comes to what kind of respirator is needed CPAP, BIPAP, or Hi-Flo oxygen NIV are all out. These systems aerosolize the virus making it almost guaranteed that anyone around them will get infected.
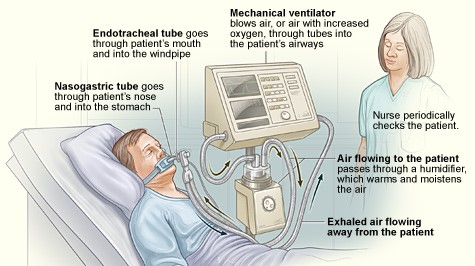
What we need is a Nasal cannula-based NIV. This system humidifies air, mixes it with oxygen and then pushes a constant stream of it into people’s lungs. If we can design a simple and working system we can give those plans to factories around the globe and get these things made. If the factories fail us, let’s also have a version people can make at home.
If you aren’t sure if a ventilator is something you can work on there are other problems. Can you make algorithms to determine if a person needs a ventilator. Can we recycle n95 masks? Can we make n95 masks at home? Workers also require a negative pressure tent for housing patients. This will be especially useful if we need to build treatment facilities in gyms or office spaces. Lastly if you’re a medical professional, can you train people how to help?
Let’s beat this thing. The ultimate medical hackathon begins.













Be careful what kind of ventilator you build, you may be putting people at risk: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30110-7/fulltext
Thank you for your input!
I just hit this page and started reading.
Could it help to have a Wiki (like the Wikipedia) as a kind of discussion and information collecting platform?
I can offer to install and host such a platform.
We may discuss there all kind of things that may help. Maybee there are any low hanging fruits more easily
collected by the hackers?
Christian
Would love to help deploy solution in Mexico, we are afraid we are going to need it soon. How can we help?
Contact me.. We are trying to build respirator from HomeDeppot or hardware stores parts.. cheap easy and hopefully could be made available to manufacture by anyone
Hey, I have no medical knowledge but an idea came to me about a vent I think could be built usign stuff we get at Home Depot. Very simply, I though of using a length 4′ pvc pipe (a liter’s worth?) to create a cylinder. A simple piston would push the air much like that used in an old steam locomotive. An electronic motor would drive the piston. Just an idea to move the air/oxygen. Thoughts?
No, majority of these designs that “engineers” are creating are useless. You NEED to have an understanding of the pathophysiology relating to respiration. Majority of these designs WILL do more harm then good. Look into Barotrauma for starters and how other legitimate ventilators work.
Hi Loppy,
Yes, Im frequently amazed at the inventiveness of engineers on this tread, but continue to spreed the message that ventilation – whether its non-invasive or invasive – is a very complex thing, involving much more than pumping air.
Designing a ventilator from scratch is difficult enough for experts with decades of experience – its impossible to design one with no experience, and impossible to build one using parts from Home Depot.
Even if one could be built, no ICU manager would ever use it, and it would be impossible to manufacture, distribute and support at a scale that would outpace the delivery of ‘proper’ ventilators made my certified manufacturers – all of which require disposables, and an expert healthcare worker to operate them.
This video gives a very good overview of some of the complexities of the physiology of ventilation …
https://www.youtube.com/watch?v=7vLPefHYWpY
We need to STOP TRYING TO HACK A VENTILATOR.
It is much better to HALVE the number of patients than to DOUBLE the number of ventilators :-
– dont be complacent
– stay indoors
– observe social distancing rules
– wash frequently
– monitor your health
– get help if you have a persistent cough, develop a fever or are short of breath
– stop hoarding protective equipment
– if you have N-95 masks, donate them to your local hospital – they need them to protect healthcare workers and save others.
That WOULD make a difference.
While I agree with much of what you said I still shudder at the thought of a hospital, doctors, hospital admins allowing someone to ventilate 4 patients with a single vent. Wow talk about cross contamination!!!
Hi Jim, I had a similar idea. Instead of the steam locomotive, how about a radial engine like the old airplanes. This would provide a smoother air flow. 3 smaller cylinders should do.
There is a safe way to ventilate with a very simple device, see this,easy to replicate no need to place a tube in the patient: https://www.hayekmedical.com/about-bcv
That is great work for people with healthy lungs, but compromised respiratory muscles – ala polio.
Unfortunately, I wont help people with severely compromised lungs that cant exchange enough oxygen,
particularly where they have sepsis / pneumonia and kidney / liver failure.
It still gets back to the issue of making something that works in volume, where supply chains are collapsing and we dont have enough people to build, test, deploy or support them.
Fromm your answers . I gather we have two problems oxygen delivery and breathing. The hayek machine helps with breathing and eliminates the need for accurate pressure and volume that plagues and complicates the ventilators.
Why not use the hayek and outfit the patient with a mask delivering oxygen no pressure or very low pressure would be needed for the oxygen portion of the solution and would simplify the delivery of oxygen to multiple patients from one source.
Other aspect to look at and has been mentioned is oxygen generation ideally the solution would have off grid variants.
Yes – but that only applies if you have healthy lungs, as opposed to lungs filled with fluid, and very likely organ failure too, where you are already in ICU and very likely on sedation and an IV line.
The problem with just a mask is that exhaled air contains aerosolised virus that infects healthcare workers, turning them into patients and causing the healthcare system to collapse, leading to INCREASED FATALITIES.
Ventilation is a very complicated issue – IMHO not something that can be hacked.
Its better to reduce spread of the disease by staying indoors and maintaining good hygiene, avoiding panic-buying, and let experts come up with the best ways to ventilate patients.
So we have to deal with breathing, oxygen , fluid evacuation , aerolizing the virus.
Healthcare system presence
Coming from the perspective of the student nurse that saved her family from ebola and used trash bags as her primary line of defense thus the initial water bottle suggestion.
Do you have a site where the timeline of the disease is explained maybe we can create/hack something that delays or eliminates the need for an “expert created device”
Hi Oz,
Thanks for your response – and thank goodness that this thread seems to be understanding that we CANNOT HACK A VENTILATOR.
We can make a MUCH bigger difference by PREVENTING INFECTION and PROTECTING HEALTHCARE WORKERS than we can by trying to reinvent something that experts, who know what they are doing, are already producing by the thousands.
https://www.brisbanetimes.com.au/business/companies/resmed-modifies-factories-triples-ventilator-production-20200326-p54e6l.html
Here is a webpage that has a good graphic of then set of symptoms – is this what you are looking for ?
https://docs.google.com/document/d/1-71FJTmI1Q1kjSDLP0EegMERjg_0kk_7UfaRE4r66Mg/preview
ELIMINATING THE NEED for a ventilator is where we should be focussing our efforts.
Hi Gary
That is exactly what I was looking for. It looks like besides prevention and boosting the immune systems.
It looks like the next greatest window of opportunity in solving the problem is the 9-10 days before reaching the hospital. By the time we get to needing a ventilator the patient has developed a myriad of other problems.
Looking at a literal heat map.
What would be the effect of heating the air around you to lets say 30+ C in ones dwellings? Are there any practical in home UV solutions? Some more questions to follow
Hope someone can answer my question. My friend created a mask which has a tube inside the mask that tube is directly connected to the intubation tube in the patient and the other side of mask has a tube that gets connected to the oxygen in the wall, which can be set a glow rate allowing g oxygen to be forced into the patients lungs. I believe they are waiting on finial approval from FDA. Wouldn’t this free up ventilators?
https://www.sciencedaily.com/releases/2010/01/100125094643.htm. Have resources like this been combed already?
Trompe – Compressed air with no mechanic parts. Can it be used?
https://www.youtube.com/watch?v=uvf0lD5xzH0
a lot of this stuff is over my head but I am good at simplifying machanical things here goes……… Could you have say two large jars of water connected by a hose on a teter totter ,pressure would be regulated by height, volume would be regulated by amount in jar ,duration would be regulated by timer? I think older ventilators used bellows but I think this would be easier? we,re talking 3rd world technology here?
Mr Teslonian built a very interesting contraption, combining a Trompe and a Ram Pump, it will generate a lot more compressed clean ambien air using no moving parts, just water and PVC pipes… Its amazingly interesting.. I’ll start to build one …
https://www.youtube.com/watch?v=xv1lQA-tnwo&t=12s
Could a single ventilator be used on 2 people simultaneously by synchronizing inhale phase and switching source with valves. between both patients so oxygen source flow is used continuously?
Actually this is a really cool idea because you could use that signal to regulate a bunch of other CPAP machines. Really the best way to approach us is find someone who designs ventilators for large companies like Dräeger in Germany – And have them attempt to convert a CPAP machine.
Yes. Using a Y piece and one way filter it can work. As long as both patients have similar tidal volumes and lung compliance AND importantly, the ventilator must be a pressure and not volume controlled one. Then you can set the ventilator at double the required tidal volume and the pressure setting will prevent baro-trauma to either patient.
Hi all-I’m a doctor and a bit of a maker. We don’t hafta reinvent the wheel. What’s needed (I don’t have the expertise) is an open-source 3D printable version of the Bird Mark 8 mechanical ventilator. They’re dead reliable, and are powered entirely by the oxygen source. As a bonus, they’re already FDA-approved. They’ve long since been supplanted by modern computerized ventilators
I think that you’re on to something with this. The system is simple and pneumatic as you said so it could perhaps be reverse engineered and manufactured from simple instructions.
https://www.youtube.com/watch?v=SG3zlpRSfWE
I just found the detailed manual for it too:
http://frankshospitalworkshop.com/equipment/documents/ventilators/service_manuals/Bird_Mark_7_-_Service_manual.pdf
Furthermore, I’ve found a lecture covering the details of the unit’s operation. Unfortunately it’s not in English so I have to make do with the text and pretty pictures. It’s a good step though for understanding the theory of operation.
I’m seeing lot’s of people jumping at electrical solutions ( my mind went there too as I’m an electrical engineer ) but we need to think really simply for a solution that doesn’t require microcontrollers or other electronics which could be a significant barrier to manufacture to many people.
https://www.youtube.com/watch?v=0OSbgqUI82U
That video was extremely informative does anyone have a basic diagram or could get something payed out so we can get to work on prototyping hard parr’s and their locations
BarryP, Are there significant differences in the Mark seven and Mark eight design of the bird ventilator? It sure does seem like it wouldn’t be very difficult to build especially since I’m sure you could call the patent on it as it’s long since expired.
https://link.springer.com/content/pdf/10.1007/BF03013322.pdf
Interesting.
I worked as a RT 40 years ago and used the Bird Mark 7 as a ICU mechanical ventilator several times. I’m pretty sure I have one stored away in a box in my garage too! The inspiration valve inside is going to be the critical component to hack and mass manufacture in order to mass produce them – there was alos a similar valve manufactured by Puritan Bennet and used on a line of PV machines. These were both pneumatic pressure limited/controlled ventilation devices – and they work well.
I think a faster and more effective design for ventilating a large number of people would be to stay with pressure limited ventilation, but to control it electrically rather than pneumatically. Basically this is the way the infant ventilators we used 35 years ago worked (and I assume they still do today.
You need to have a source producing a continuous flow of air/oxygen at a source pressure great enough to inflate sick lungs (around 30-40 cm H20 pressure) and at a sufficient flow rate to inflate adult lungs – around 750 cc volume – in 1-2 seconds then all you need is a way to control a valve to open and close at an adjustable rate (i.e closed 2 seconds, open 4 seconds, closed 2 seconds, open 4 seconds …. would result in ventilating a pt at a rate of 10 breaths/min).
Just imagine a length of rigid tubing 4 ft long running from left to right. At the left end is the air flow source (compressed air/compressed 02) – the air flow would need to be adjusted to approx 350cc/sec – at the other end is a valve that closes for 2 seconds then opens for 4 seconds. In between the two is a hole in the tubing that is attached to the patient – just imagine a balloon/test lung attached in the middle. When the valve closes , pressure builds in the entire tubing circuit and the lung inflates, when the valve opens the pressure drops and the used air is expelled out of the opening created by the open valve (and gets routed through a filter to prevent particulate aerosolization).
We have lots of sources of pressurized air and O2 available – the tubing circuits are already readily available – even the valves already readily exist in both disposable and reusable versions (the most readily available ones use a small volume of pressurized air to seal/unseal a diaphram. So all that would need to be developed and manufactured is an adjustable controller to open and close those valves.
Perhaps even more importantly if large portable hospital/treatment facilities need to be setup – a single high flow source of compressed air and o2 could be “piped” to multiple patient treatment sites – there something to limit the compressed air/02 flow down to the flow rate necessary for each individual patient – could be as simple as a fixed orifice – would be necessary – then you just need the circuit with controllable exhalation valve described before.
Lots of custom machined parts; cross section here: https://thoracickey.com/how-ventilators-work/ You need the drawing package. Vyaire is the current vent company out of many over the years that swallowed Bird
Great idea about the Bird. I haven’t seen one of those in 35 years.
How about taking a manual self inflating bag ventilator (AMBU) and constructing a detachable pressurized cylinder around it. Use an Arduino and several solenoid valves to make a pressurized “bag in a box” style of ventilator. This would also create a closed system that would reduce cross contamination. Put in some flow and pressure sensors to feed back into a timing loop in the arduino to cycle a breath.
The automated AMBU has been done – see these links.
https://patentimages.storage.googleapis.com/22/ce/16/6fb96f2bc99ff4/US4620538.pdf
https://oxvent.org
That oxvent is what I had in mind and would be a great solution if they can get it into production.
Yes – it looks that way at first …
But what is the point of building something that generates compressed air when it is powered by compressed air ?
Ambu bags are used to generate compressed air in an emergency when there is no other source of compressed air available, and/or when the rate and depth of compressions need to be tightly controlled by a HCW based on the patient’s individual conditions and response to treatment. The HCW provides the feedback loop.
Compressing the Ambu bag is one thing – but controlling the rate and depth is a different matter.
hi Dr. duel i too am trying to add ideas to help wid making ventilator parts….thus far i have these ideas recycle wheels off office chairs
and make the wooden x dolly for the moving
unit
use flexi arms off of the study desk lamps for the hanger wire for hanging the tubing
use tubing from pool supply stores
and tubing from fish aquariums oxygen generators…we could also use corn remover
band aides for grip to hold the nasal cannuli on the face….the thing is Dr. we can
do fundrives for these parts but
who will collect the stuff who will ship
who will assemble? we can repurpose
stuff to make ” parts ” but we screwed ourselfs cus china makes every aspect of the device…we don’t need hack athons
we need the raw materials to be sourced
here in usa also the plastic caps on water bottles is the type of plastic to make tubing
not the plastic of the bottle itself…
the molds to make masks are sooo
propriety intellectual so we need to
put the design patens aside for manufacturing. just to collect
4 wheels for 30,000 ventilators
is 120,000 wheels can we scour
every salvation army for office chairs
to that many? who can buy up
used office chairs and tear them apart only
prison labour. each state would have to chip in
2400 per state used chairs for the endeavour.
we could hijack thin coat hanger wire
as a backup for hanging the tubes thats
600 coat hangers per state.
Hello! a group of local engineers managed to reverse engineer this machine with a few updates. Total cost around 5K able to be produced with commonly found industrial components (PLC based) no hobby servos, no cheap arduinos involved. This machine is designed to run 24/7 for weeks
https://www.facebook.com/crafters777/videos/1149599925374335/
You got to understand, Most Nurses do not understand respiratory in a meaningful way, especially in the very ill! It is a Respiratory Therapist that runs the ventilator and understands pulmonary disease.
I am a retired CRT that worked as a Respiratory Therapist for 35 years from 1981.I worked with Bennett PR-2 ,Bennett MA-1,Bear-1 &2 ,MA-2 ,and the 7200 back at Edgewater Hospital before it closed.I was wondering if any of these “vintage” ventilators are still available for use during this time?
I am a critical care MD and have looked at what they are using in Italy. They are using ventilators on the very sick but many more are being treated with a simple CPAP machine hooked up to a crazy looking helmet.
This helmet is a special type of “Interface” that connects seems to be working very well. It is virtually unheard of in the USA and to my knowledge, we do not have them. Though ventilators are important, the large manufacturers are gearing up to make as many as they can. The problem I foresee is this type of interface.
I would love to challenge the maker world to consider working on this.
Check out this link
https://www.youtube.com/watch?v=2eCMUzYM3KI
Hi Doc, sounds like something interesting-the helmet-30 years never saw that type thing either, so design wise it needs an inlet to a BIPAP/CPAP which hopefully has demand type flows, and then an exhalation valve thats separate or part of the input, somehow everyone seems to work a bit different. but the exhalation is a spring loaded plug valve or could be water submersion ( but probably not) . We tended to shy away from full face mask due to possible aspiration, if someone vomits, and they always do, how do keep them from inhaling the stuff and causing more problems, so what ever anyone does, make it so easy to take on or off
also keep in mind, we put this on someone trying to keep them off a ventilator, if we fail we end up loosing another resource
It’s not much different than what beginners use for Spray Foam Fresh Air supply. I’m unclear what the PEEP valve/adjustment does. Any thoughts? Is that regulating how much pressure stays in the hood and is measured in Water Columns with the simple Manometer?
PEEP is gonna be huge for these patients. PEEP is the pressure exerted on the smallest airways – the alveoli. PEEP recruits these small airways to remain involved with oxygenation. The covid patients that require these procedures are super hypoxic due to the alveoli not being involved in oxygenation due to fluid/inflammation and the difficulty diffusing oxygen through this fluid inflammation. The PEEP (normal is 5 and I’ve been told many of these patients require 15) is increased and helps drive the supplemental oxygen through the inflammation/fluid. So, you could have all the ventilators in the world, but if you didn’t have a way to turn up the PEEP it might not help in most of this population of patients.
By the way, to the guy that said nurses aren’t smart enough to manage ventilated patients….I beg to differ….
NBC news showed this story that offers a USA + FDA Approval…
https://www.nbcnews.com/news/us-news/texas-mom-pop-business-flooded-orders-helmet-ventilators-amid-coronavirus-n1173466
He is offering to make the plans available to people…
Hi, I have been thinkin in an arrangment that could be brought to prototype. Starting with an electric motor, variable RPM control, to this motor a shaft conected, to this shaft, are conected diferent types of barrel cam discs, (pear type, double, tripear, etc) thus giving in the same single rotation of motor multiple pushes by single cam disc, (each cam conected to a clear tube with a pinston in it, to valves, intake and exit, each piston can be used individualy or multy exit. the volume displaced in pistons should be the same as in respirators. if needed it can be used in reverse combination of valves as to inhable and exhable. if someone finds this not to be rubbish, my grain of sand.
Idea comes from swash plate adjustable compresors. and cam folowers in kinetic design,
PD, if theres a chance to place image?
Regards,
Martin
I think that helmet mask interfaces have been used for Non invasive ventilation. I see that the oculus virtual reality device is also a helmet mask design . Facebooks oculus manufacturing should design a lot of helmet mask devices . They already have a manufacturing facility in florida
Want to recycle masks? Here’s a Chinese study saying that 30 minutes in an oven at 70 degrees celsius will do it: https://mp.weixin.qq.com/s/3QYVWO4kj5qwuSHnhcM9uQ
This was posted on FB today:
As some manufacturing supply chains are on hold due to Covid-19, hospitals in Italy have used 3D printing to save lives. The Italian hospital is saving Covid-19 patients lives by 3D printing valves for reanimation devices. At the time of the report below, 10 patients are accompanied in breathing by a machine that uses a 3D printed valve. In the background 3d printing enthusiasts have also created an online platform to help support the medical supply chain, Search “OPEN SOURCE COVID-19 SUPPLIES” through Facebook and they have a group if any of you would like to view.
The link for the article is below:
https://www-3dprintingmedia-network.cdn.ampproject.org/…/a…/
Your link is nog working…
Try this one
https://www.3dprintingmedia.network/3d-printing-unite-for-covid-19/
Great community!
I work as a production engineer for electronics. Two weeks ago I thought that industrial countrys like Germany will have all the machines and ressourcen to build any equipment that might not be perfect, but save lives.
The main problem will be to setup groups of companys, that invent or build a solution with things we – or even better- almost everybody has.
Don’t know…. Using vacuum cleaner motors, filters and tubes adding some drill Maschine controllers. *Justabrainstorm*
Maybe the government should force the medical companys the publish there construction plans, so everybody can rebuild the machines with things they have.
That’s a good start. Someone had made a comment about using a centralized air system to force air into many units for a field hospital. I wonder if a standard air compressor (or for a smaller setup, maybe a tire inflator?) would work.
Most hospitals have pressurized air already available, and MANY times more outlets for air/O2 than available ventillators. Look at the BIRD Mark 7 for inspiration. It runs entirely off pressure from the wall. If you can come up with something similarly simple but able to run a modern ARDSNET ventillation protocol you’re heading in the right direction.
I found this thread because I’ve been kind of obsessing about this stuff and possible solutions given my experience w/ med equipment in clinical engineering (field tech), anesthesia (tech), time in the OR, yadayadayada. After posting to a similar forum/crowd-source question in JAMA re: reuse of PPE (in the OR we have 3 main sterilization options for ad-hocs: steam (autoclave); the Steris machine (liquid solution, automated circulation, main use is for scopes – bronchoscope, colonoscope, etc) and “the (very dangerous!) gas”: ethylene oxide (EtO) – posted a ref. to a study from .. some prior event that involved a shortage – reputable source/journal .. focused on EtO as an option as EtO was the 1st thing that came to my mind…. anyway, the BIRD is the 1st thing that came to mind re: resp though my experience with them is limited, they did the job back in the day alright – and in no small way contributed to Forrest Bird receiving the Pres. Freedom Medal before his passing in 2015… those little green boxes used to be everywhere (where have they all gone?!) and indeed ran on the pressure of the O2 coming in – and all mechanical. Another thing to consider is replicating his earlier-than-the-Mark-7 designs he had from making them from scrap, basically, out there on the battlefield as a medic – the very basic function of course, and I don’t have a clue as to what minimum functions you need from these things (someone said the 8s are quite different – but don’t know if the added functionality on the 8 compared to the 7‘s basic functions make it usable for this application and the 7 not usable – or maybe that’s not the case at all – and either could be used?) but my gosh, I can’t think of a better road to go down given the dire situation & massive gap btwn demand & supply… all mechanical, simple dials, no electronics.
I read the post about the Bird Mk 7 and all those, yes they are simple and no electronics, yes-if you know how to work on them-you can do it, but they were pretty finicky, they work with magnets, and have a piece called a pneumatic clutch, so unless you have one to work with, its not as simple as working from a picture. the power of the magnet, its size all effects how it performs
if you want an option look at the PR2, its more pneumatic and has a simpler valve, its a vane that rotates, uses a ruby crystal to reduce friction
I was a Navy hospital Corpsman, also worked in operating room as a surgical technician With regards to resterilizing the N95 masks. I agree with above comment of Ethylene Oxide gas. We used it for everything that couldn’t be steam autoclaved. Also consider Steris, it’s a hydrogen peroxide system which is used for cameras and other delicate equipment. I’m.sure it would work well for the N95 masks. Cidex is another option we used this when all the steris machines were in use. It’s a liquid that is safe for cameras and scopes also anything that was usually gased could be cidexed if needed. It takes about 15 minutes. While I was working in Austin, early 2001 the OR used a reusable surgical gown, back table cover and basin liner, not sure what company but the gowns were resterilized and came in a cloth wrapper. They were made out of a parachute like material and were fluid resistant. I had another idea that could work. If you had a clear barrier over the mask something that could stick to mask. You could potentially change out just the barrier and wipe down elastic part of mask with clorox wipes or similar product.
Hi Denise,
There have been a lot of conversations about sterilising and re-using N-95 masks.
While sterilisation might be able to kill the virus, it wont be able to remove the spit and mucus that accumulates in the mask.
If you washed the masks, that would almost certainly reduce their filtering ability, because the microfibres would be disturbed – a bit like a wool sweater shrinking in the wash. Some masks are based on electrostatic effects (esp the best ones), which are very likely to be destroyed by washing as well.
Cameras etc that are sterilised using Ethylene Oxide are first given a thorough mechanical clean using other sterilisers, to remove biological residues. You can’t do that with a mask.
Some masks have a separate filter, which would almost certainly be destroyed by washing – if washing them is possible.
I’m not certain what the sterilisation process would do to elastic straps.
All this means that a mask made to the N-95 standard couldn’t be guaranteed to provide the certified level of protection after being cleaned. So – it would no longer be N-95, but something less, plus a risk of being infected already.
Even if a mask could be safely sterilised, one has to think about safety issues associated with the workflow – handling contaminated masks, transporting them through the healthcare system, cleaning and sterilising them, shipping them to the point of use, and the risk that some virus might have survived the process. It would almost certainly cost more to clean a mask than to make new one.
The production of new N-95 and equivalent masks is ramping up at a rapid rate – better to use a new mask with known performance, than something previously contaminated.
Gowns and drapes are different – they’re designed for high-temperature cleaning, have no 3D form, no elastic – they provide a barrier only, and don’t have a filtering function.
Here is a useful paper from the National Academies of Science, Engineering and Medicine … (from 2006)
“Disposable masks and respirators do not lend themselves to reuse because they work by trapping harmful particles inside the mesh of fibers of which they are made. This hazardous buildup cannot be cleaned out or disinfected without damaging the fibers or other components of the device”
“Reuse of Disposable Medical Masks During Flu Pandemic Not Recommended; Reusing Respirators Is Complicated”
https://www.nationalacademies.org/news/2006/04/reuse-of-disposable-medical-masks-during-flu-pandemic-not-recommended-reusing-respirators-is-complicated
And from Forbes
https://www.forbes.com/sites/brucelee/2020/03/30/reusing-n95-masks-against-covid-19-coronavirus-the-risks-and-options/#3d6e6997df7e
The only real solution to the shortage is to support manufacturers to ramp up production of >certified< N-95 masks as quickly as possible – and to destroy used PPE via existing infection control workflows.
I am an air compressor mechanic, I would not want to breathe the air coming out of the vast majority of them. It would need very good inlet filtration and be oil free, at the very least.
Hi medical grade compressors run oil free
Seems like you might be able to modify a CPAP machine. There are a lot of those out there.
I think the implementation of a midi clock (music equipment) could be used to trigger your vacuum idea. If the mechanical elements were assembled, it could be triggered by a laptop or drum machine and then use the vacuum motor to fill the lungs with air. There could be a separate device that is triggered by back pressure to release the co2 from the lungs.
I know nothing about ventilators or engineering but I think there is something to be explored with the incorporation of midi being the clock.
. I thought I might share my idea.
Just a tiny bit of background, I am a retired (to a small town in Italy) aerospace Project Manager/Risk Manager/Flight Test & manufacturing electrician, but my passion has always been motorsports. I’ve built race cars, won races as a driver and owner, etc.…
My idea, and I spent some time two days ago proposing this to the world’s top racing organizations, is to harness the power of these organizations to help with the problems we currently face with our medical manufacturing infrastructure. Nascar, F1, IMSA, FIA, ACI, FIM, WEC, Indycar. So far, no response.
Put the drivers on iRacing, and put the rest to work helping with these problems. Give them season points for production of units.
Carl Haas (US) has the engineering and manufacturing prowess in his groups alone to probably singlehandedly solve these problems. You can add 50 more names to that list. These are organization that are highly flexible and you will find no group of professionals, and amateurs, that can be more single-mindedly focused on a problem or goal than racers.
Just think if your grandpa could have a ventilator designed and built by Mercedes F1. Anyway the PR and marketing opportunities for these organization are endless, but that is beside the point. I see no downside.
If necessary I may see if it would be feasible to take this grass-roots. For every one person working in professional motorsports there are 1000 or more doing these things for fun with similar skills and attitude.
Meanwhile, I’m going to be looking at the technical requirements for a ventilator, how difficult can it be.
If you could help get the word out, or if can help with this issue some other way please let me know.
Let’s kick this things ass!
Best Regards,
Daniel Curtis
How to get oxygen? WATER IS FULL OF IT! If you have electricity, you can have oxygen. make on site. electrolysis!
Same idea. But how to make sure, that there comes nothing else with oxygen. Water must be very clean, I guess
Distill the water.
Distilled water.
That’s a very energy intensive way to get oxygen. Oxygen concentrators are much more effective and energy efficient.
About preventing coronavirus. We can make converters for buttons in lifts, trams etc. to make them contactless. I think there should be 1 module for 1 button (for compatibility with every buttons panel): on the front proximity sensor (i. e. capacitance sensor or, where there’s not much sun, optocoupler), on the rear electromagnetic mechanism pushing the button, and also some powering cable (low voltage DC). It can be mounted i. e. with cyanoacrylic glue.
For opening doors, there could be pedals mounted on their bottom edge to unlock them (connected with knob by some string) and push or pull them by foot.
Howabout just gluing extensions on them so they’re easier to push with your tongue…. okay elbow.
And a sign, do not touch use your elbow! Or something to that effect.
Also a uv tube or some way to continually minimise bacteria on the buttons/extensions
it could be dangerous because of scattered radiation (direct too, if it doesn’t switch off when someone touches it) and produced ozone
a Lot of folks that have had eye injuries or defects have high UV sensitivity, exposed UV lights can literally blind us to areas.
if you want to ensure i cant see the buttons to press them, shine a UV light on them, the panel becomes a brilliant opaque ball of almost voluminous purple/pink lens flare.
– Set the UV lamp to RUn when the carriage is empty only.
Why not just have people adapt to carrying a stylus for pressing buttons in public? They would be a little larger than those used on iPads and the like.
Just need a few lessons from an OCD sufferer.
Do NOT use your hands or fingers to touch anything. Other people have been scratching their arses or going for a shit and not washed their hands. Then they touch buttons and poles on buses and whatever else. NO! We use our elbows or our sleeves.
If you really must touch something dirty, use just one hand. Keep the other clean for eating and touching your face, etc. You will keep a constant mental log of which has touched what, where. Of course the principle carries on. If you use your elbow to touch something dirty, your elbow is now dirty, so don’t touch that.
Wash your hands as soon as possible, in the proper medical manner. There are diagrams of it near every sink in every medical facility I’ve ever been in. Soap and water are fine, you don’t need anything stronger. Except don’t use soap cos, fuckin’ hell, people touch that after they’ve had a shit! Use liquid soap, and of course, operate the dispenser with your elbow. Same with the taps, no point washing hands then re-dirtying them on a filthy tap.
There was that maternity hospital in the 1800s where they saved hundreds of lives by getting the doctors to wash their hands. Between visits to the mortuary to fuck about with corpses, and delivering babies right out the flange, and touching all that delicate receptive tissue with corpse-filth on their hands. Soap and water are really your best friends as far as germs go.
Nothing wrong with hard soap, if it’s really soap, there was an awful lot of “moisturising beauty bars” that were basically a fatty banquet for germs, but proper soap is fine, everything on it will be dead.
Oh wait… for the switches, I propose beam-breaking. With the beams nice and far away from walls and other surfaces to there’s no touching anything. Use red laser beams, or any other colour, but make sure they’re visible. Or else, yep, foot pedals. Except people who can’t walk would have difficulty using them.
We could make a touchless world. Except for the things we want to touch, of course. Wouldn’t take long or much money, just replace switches with touchless ones as they are due to be replaced. The public would get the idea quickly, and it would be a bit like Star Trek so they’d probably think it was quite cool, and an innovative solution to a public health problem. A politician could reap a lot of credit for getting some switch manufacturer to do this. And he might have bought shares in their parent company through a number of shells of his own, so when they get the government contract, quids in!
That, and giving everyone OCD, would save many lives I think, in every epidemic to come. Currently I’ve survived about half a dozen pandemics without so much as a sniffle, I’m obviously the bastard son of John Wayne or something.
Just use a tissue when pressing buttons or panels.
But also a glue on paddle for standard commercial as well as domestic light switches so they can be operated with elbows instead
https://www.instructables.com/id/The-Pandemic-Ventilator/
air valves can be found in broken medical pressure meters (some are NO, some NC)
In fact, the PLC could be replaced with arduino together connected over OTG and supply data to tablet or old phone running an application which can record the data and would contain the controls.
What about plasma filters? In hvac you can install these in the blower compartment and they claim to destroy 99.9% of all viruses. They are used in many hospitals. They are only 24v but can be 120v also.
I don’t understand or know the equipment of what these specific ventilators are but I do know that I have used aquarium pumps to push air through wort, adding oxygen to the liquid for fermenting. If you just need a way to push oxygen in a mask and zap the air to kill viruses maybe something could be done with these components.
Again I don’t know much about this medical stuff but I just want to throw in some apples.
Did not expect another home brewer to be in the comments here. That’s a great idea with the aquarium pumps. Along the lines of a mask that filters (and aquariums), activated charcoal is great for a filtration and pretty much can be made by just burning clean wood. That would be for an area in a supremely sorry state, but it’s feasible.
Technically you’re not burning the wood so much as putting the wood through an anerobic pyrolysis reaction. You need semi-specialized reaction chamber (or loads of extra feedstock) and the clean wood also needs to be bone dry. There’s a whole community of people doing home made charcoal/biochar who could probably supply a crapton of charcoal that would be about 75% of the absorptive capacity of activated charcoal. I’ve been researching this stuff for a carbon capture project but have zero hands on experience with it.
The specialised reaction chamber was historically made out of mud piled over a well established fire. Research traditional charcoal burning for rough and ready methods to get it done.
I like this idea — my first stupid idea was using scuba gear and a dairy milking machine for ward sized deployment :p I am not sure at all but the most effective use of resources in the short run might be pooling / registering all ventilators and suction units from dentists offices, plastic surgeries, orthodontists, vets etc. etc. Maybe all oxygen, compressors and regulators from scuba companies. Perhaps make a local registry system through professional associations and hopefully companies will donate or loan to front line ICU on an as-needed basis. Big IF is if he equipment is comparable / usable by ICU procurement. Deployment logistics and inventory control is a cinch: there are a ton of roadies and trucks available right now since everything is cancelled. They are experts at moving sensitive equip. If this is a good idea shoot me a line at devon@ostrom.ca
Someone has already started working on this here: https://www.lesswrong.com/posts/LwcKYR8bykM6vDHyo/coronavirus-justified-practical-advice-thread?commentId=7NiWw3PbjQS8ZuYAR
Pasting for convenience, but credit to Mark Xu.
———————–
bipap + O2 concentrator + capnometer + Y juntures + tubing
– https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/bipap
– https://www.wikiwand.com/en/Oxygen_concentrator
– https://www.sciencedirect.com/topics/nursing-and-health-professions/capnometer
You probably need around 5L/min of 90% O2, which theoretically requires a medical grade condenser that requires a prescription. I, however, see no reason why getting 5 normal O2 condensers that can deliver 1L/min of 90% O2 and connecting them all with Y junctions won’t work.
[Edit: you can probably do with 4L/min of 70% O2, so you’ll need 2 O2 condensers. This advice is mostly based on priors and like 20 minutes of research. The crucial point is that you’ll likely need at least 2 O2 condensers]
These devices should all be relatively easy to use. Many people use a bipap for sleep apnea. Many people with respiratory problems have their own O2 condenser that they use. The capnometer I’m less sure of, but there should be a simple flow chart on what to do. If there isn’t, I will make one by talking to doctors.
The reason you need the capnometer is because giving people too much O2 also has its own host of problems.
The total cost is about 2k for the bipap, 5 * 400 for the O2 condensers, and 1k for the capnometer for 5k total.
Hi , a long time ago worked on ventilators that used fluidic logic as control. The model I think was a Monagahn 225. It was completely powered and managed by the oxygen / air supply. Aside from being interesting tech I haven’t seen for years it would seem to me a solution ideal for fast production using 3D printers
about fluidic logic : https://www.symscape.com/blog/fluidic-logic
sources of inspiration ( sorry about the traffic Frank) http://www.frankshospitalworkshop.com/equipment/ventilators_equipment.html
I don’t have a 3Dprinter but someone out there may be inspired, here’s hoping
Two things this morning:
Thing one, Sticky this thread let’s keep it up top!
Thing two, instead or reinventing the wheel…how about we look to the old expired medical equipment that the patents have expired? Or just for ideas that HAVE worked and HAVE passed the regulation process? For example:
https://patents.google.com/patent/US3191596
Just saying, short cuts at this time would be a benefit.
A reply to my own comment:
We need a few things:
A repository for the plans, documentation, schematics, and a location to have parts assembled and distributed. If we go the rout of 3D printed parts we need to be able to download the .STL files? Printing instructions? I think https://www.thingiverse.com/ may be a good place to upload files to.
Documentation:
For the regulatory folk here:
Needs and wants
Risk analysis
Low Level Requirements Specification
Requirement Specification
Functional Specification
Test Plan
This may be at a min. what would help keep us all on the right track. Let’s get moving on a plan!
Regarding “Can you make algorithms to determine if a person needs a ventilator.” I suggest that existing dataset is published on kaggle.com where people with right skills are available.
My thought was to use a computer case fan, a fan controller chip and an arduino. I’m thinking the case fan can quickly speed up and reverse.
Fans in general, even server ones, make insignificant amounts of pressure against any resistance. Centrifugal blowers do a bit (COTS ventilation type) to lots better (When specifically designed for it)
There is also this one for a guy at mit. https://github.com/nikaiser/openVentilator/blob/master/MIT%20Low%20Cost%20Ventilator/Ventilator%20Video.AVI
From 2010:
https://phys.org/news/2010-07-students-low-cost-portable-ventilator.html
There’s a Chinese DIY one here that allegedly worked… I doubt how many certificates it would get, but the guy using it is at least still alive.
Time to join an internetional effort, see #projectopenair.
Sorry- forgot link to earlier post:
https://www.dailymail.co.uk/health/article-2270178/Chinese-man-kept-alive-years-HOMEMADE-ventilator-family-squeeze-18-times-minute.html
It was to show that an extraordinarily crude design has actually kept someone alive, according to the report..
A Different Kind of Design Approach to Solve the Problem at a Different Level…
What is the fastest path to saving lives: a new/better design, or a design for how to get resources to scale up production of already-certified products that have already-existing production facilities and supply chains?
I have run medical technology companies, though not one in this area.
Would like to offer a third, different alternative than the two main perspectives that I see represented thus far on the thread.
Existing perspectives:
1) We need to quickly design and build (or repurpose) an adequate machine to save lives. Saving lives is more important in a potential massive loss-of-live emergency than money, or the law, or liability.
vs.
2) We cannot quickly design and build an adequate machine because it is against the law due to licensure and other legal requirements. BTW, in most countries that’s both orange-jumpsuit-in-prison criminal law, as well as personal bankruptcy civil law.
Question to bring this home: would *you personally* sign up today to go to prison or to go bankrupt to illegally provide a device to people to save their lives? Maybe there are people who would… but it’s a very tall ask even in a loss-of-life emergency… and it’s a real possible outcome.
I’d like to propose a third way forward, which I believe may be the most effective ‘design’ hack:
3) Design a process to rapidly fund and scale up production and distribution of already-existing, already-certified technology, and to train people to use it.
A) Raise the money. Many people want to help, for altruistic reasons, profit-motive, or through government. There is substantial opportunity for raising funds from small or large private donors (yes despite the current economic conditions), from foundations, from insurers, from companies, and from government sources, though getting this to happen quickly may be a great challenge. Some creative ideas for more rapid funding:
i) Crowdsource funding, either through donation or some form of purchase.
ii) People pay in for a ‘subscription-like’ service that raises monty to build technology to be available for everyone, and the individuals who pay in money get priority access to technology if they ever need it.
iii) Allow an ROI to individual investors, small or large, who loan or invest in production with the hope of a financial return
iV) Look forward to other ideas. ;-)
If the cost-at-scale of existing machines is in the low thousands of dollars or less, and each machine can save multiple lives, the financial case is *already* extremely compelling, even with existing hardware designs and price points.
B) Focus on design / process engineering to dramatically increase the throughput of production of existing machines, and thereby the number of units in the field. Work with existing manufacturers. This is likely a rate-limiting step initially, and could be addressed nearly immediately.
C) Design processes to train personnel to use the equipment. This is likely a rate-limiting step later.
Finally, another approach:
4) Get at-home or in-patient oxygen concentrators to people to decrease the number who ever end up requiring ventilation. Supplemental oxygen, especially at home, is dramatically simpler, cheaper, and safer. Other approaches can decrease the likelihood that people ever need a ventilator.
Question to appropriate specialists on the thread: to what extent do you believe that early administration of oxygen would decrease the incidence of patients presenting who ultimately require ICU care, ventilation, etc? Would this be an appropriate way to take the burden off of downstream systems?
Thank you to the creators and contributors on this thread!
Looking for ways that everyone who wants to can contribute to solving this humanity-level challenge…
The UK. Government is asking for general manufacturing like JCB to switch production to ventilators. While light on detail I assume it will be a licenced design with certification. It is relatively easy to do that, and rapid tooling for plastic parts, CNC machines and other processes, when applied to proved designs with existing manufacturing details, can make production parts in days, if not hours.
What is not used in UK could be export.
That is the way to do it in the west, and actually few nations lack similar resources if they so choose.
Hi Christopher, I’m liking this approach. Could you let me know if existing manufactures we could contact.
http://www.onebreathventilators.com/
Company that already developed less expensive ventilators, http://www.onebreathventilators.com/
Article describing cost and manufacturing risk issues, a bit similar to Christopher’s points, https://www.technologyreview.com/s/615380/we-need-more-ventilators-heres-what-it-will-take-to-get-them/
I think this unit when available ( testing phase and waiting for someone to consider approving it) would be around 4,000 dollars. Cheap by comparison to hospital ventilators.
I have contacts in Mexico and we could manufacture here. No problems, I also have been working on medical devices for a long time…. I’m in
same mit design:
https://www.fastcompany.com/1661942/mit-students-invent-100-ventilator-for-disaster-zones
There are some great ideas and a lot of impressive talent on these posts.
This looks very promising for this design. At 100USD per unit, you do not need to sterilize, as long as there is no issue for the first use. At 100USD, it will essentially be personal and disposable, after one use. The component parts look to be very simple, cheap and readily sourced. Could build from Home Depot and Radio Shack\Frys\Grainger.
At end of use, dismantle, remove virus on some buik parts to recycle, but not put back into service for another ventilator. The rest are burned, etc.
Can we commandeer engineering schools schools to have students build these type of ventilators and publish the continual innovations as they are discovered? If you want a valuable education, build 1o to 20 of these, each. Make the Mech Eng and Elec Eng departments as the factory sites.
There are 387 Engineering schools in US. At 5000 ventilators per school that would be roughly 2Million ventilators at 200M USD. At best, there are 100,000 ventilators in the US today.
So, ideally, the ventilator solution would be staged.
1. Most acute and critical – use the reusable mechanical ventilators at roughly 100,000 units in US.
2. Next wave of patients that on edge of critcal – CPAP machines paired with a device to meter O2, if needed. Might not be reusable or able to be fully sterile. Although, if it is a patient who already has the virus, we may be able sterilize as best as possible and reuse. Good benefit for CPAP is there are already capabilties for monitoring of patient online with these devices. These cost about $500 to $1000 USD per unit. I own a CPAP and they have more controls than the 100USD ventilator device. There are roughly 3million users of CPAP machines in US. I do not know what is the immediately available inventory of these machines. This may cover all that is needed.
3. Mass use and disposable – Use the 100 USD disposable unit. Last line of defense. Could be used for mass wave of patients. Make as many as needed to fill final capacility needs. With this anyone will be able to have ventilation, if needed. This device might not be needed in US. We should certainly partner with others to build if needed for other developing countries.
Forget the 3-D printed stuff – it takes way too long to manufacture and how do you sterilize plastic? I have a complete machine shop and can make stainless steel components faster using a “real” CNC lathe or mill. I can weld SS if I need, to down to 15-thousnaths thickness. Complete quality control, heat treat, sterilize, and packaging available
that part would print in 1 hr … and stick it in oven for 30 mins at 70 deg … to kill bact
Maybe you could contact
https://www.3dprintingmedia.network/3d-printing-unite-for-covid-19/
Alright. Think outside the box with me. We modify 3 axis 3d printers with heated build plates. Use the x axis as a breath bellow, the Y axis as an exhale bellow, the heated build plate as a water warmer for a humidifier, and presto. After designing the bellows and routing the tubing you have it. All temp, speed, volume can be controlled with a modified slicer program. Add a ozone generator for the exhaled and contaminated air and you can keep the infection from spreading to everyone else.
Just my preliminary thoughts.
Thats a clever idea !! I like out of the box ideas…. I was thinking ardunio controlling air compressor frankinstin with oxygen tank ….. however I could see how yours could be implemented … i’m going to post your comment onto a 3d printing fourm to get the word out .. never know …. i’ll post in here https://www.facebook.com/groups/prusacommunity/?ref=nf_target&fref=nf
All the objections here are easy to overcome – Doctors define the parameters, engineers and hackers find the hardware to meet those standards. You don’t have to be both. Teamwork.
The Bird ventilator was the industry standard for years, and the first items -delivered- to hospitals were made with bakery tins and a repurposed doorknob. They replaced a British unit using a car wiper motor with the arm inflating and deflating a bellows.
It does not have to be complex, but it does need to be defined by medical personnel. Only once defined can we see the challenge we have to meet.
Organizing that team is the first imperative.
UK input. All fighter planes, pilots, commercial planes have oxygen masks. Commercial aircraft use one time oxygen generators for emergency decent. There are oxygen masks for passengers. There are thousands and thousands of these tgat may be able to be repurposed, and the planes are not flying. Aircraft could be repurposed as isolation units, and oxygen connected externally. They already have ventilation that runs from ground power. Serious cases could use the military head gear.
Also, the planes could be flown to local airports where there Is critical shortage of isolation units with oxygen capability. Only the most urgent cases then use hospital ventilators.
Looks like they are working on some variations of this project in other places as well:
https://www.instructables.com/id/The-Pandemic-Ventilator/?fbclid=IwAR131d8iY_9xtpTzqYjyKtDzW0lVELJy5ZIyklg1vtuDIXK0o46Yiil7M-k
https://panvent.blogspot.com/
https://app.jogl.io/project/121
I’m sure there are some good ideas that can be built upon from there.
Checkout this project https://app.jogl.io/project/121
It seems to be a very well organized approach!
Hi all.
I’d like to help on this project where possible Here’s my thoughts.
Firstly, A significant political proposal : Petition to invalidate Patents on ventilators for the period of 2020. Companies that produce ventilators should release their designs now to allow swift, mass production. On a domestic level, that information would assist in a “People’s Ventilator Specification”.
To “The People’s Ventilator” – a proposal of list of project objectives / specifications.
1. A significant proportion of humanity is facing a real existential threat over the coming weeks and months. At this point, profit and regulation becomes a clear second to survival. My strong feeling is that this should be approached as a proposal for “A People’s Ventilator” – not a commercial product.
2. Regulation has some very useful information – it is not designed to hinder production. However, we do not have the time to get the rubber stamp of certification. But we should use the compliance information to construct the principal specification and guide testing.
3. I propose this project being considered as an open source / free to build kit of parts, using off the shelf parts where possible. All designs should be open source and complete.
4. 3D Print as much as possible – Although not ideal when compared with skilled manufacture or vacuum form as suggested by Eric, 3D printers have become common world-wide. They represent the fastest way the majority of people can reliably manufacture parts consistently. But keep the designs simple – easy to assemble with minimal part quantities.
5. Materials. Aside from 3d printed parts, we should try to use commonly available materials. I haven’t looked at the detailed makeup of a ventilator yet – but I think it would be beneficial and most effective to look at materials easily available. As Eric mentioned above in an earlier comment – the using of scooter wheels for hospital beds was a very effective volume solution that was also cost-effective, versus custom manufacture We should try to using commonly available parts. For instance, could we use material from air-beds? (Just trying to set a perspective of thought here)
6. Reliability and interchangeability of motors . We need to find and test as many motors from common devices. Work out how can we make them run 24/7. The motors should be detachable and replaceable – so 3d printed designs should have an externally mounted motor to allow available parts to be fitted. Power and speed control should be determined by the controller during an automatic calibration process for new motors. We can also monitor the temperature of motors and have a settable acceptable temperature.
7. Interchangeability of high-wear items. Similar to 5 above, we need to identify high-wear items and ensure they can be easily reproduced and easily replaced.
8. Cleaning of parts – the ventilator should come apart to be cleaned regularly. A simple method of cleaning, proven in a lab would be useful to ensure we can re-use ventilators. (anyone got a lab who can test infected parts?)
9. Controller – Arduino / Raspberry Pi control – these are globally available, cheap and many people are deeply familiar with programming and interfacing. Avoid use of LCD screens as a critical component. Keep it simple. Use LEDs (which are available in abundance) to display statuses and keep software simple.
10. Software – A State-Machine approach. It should monitor sensors and control the flow of air / humidity in a State Machine format. It should be configurable to and principally self-calibrating to allow for variation of parts (e.g motor control). Choose a language easily understood by people. Keep it well structured, over-commented and strictly to a ‘fail-safe’ state machine design. Good naming of variables, etc will be essential to allow as many people as possible to read the code and contribute ideas.
11. Split ourselves into a series of ‘teams to focus is on those specifics – Project management and Principal Specification, 3d design, electronics, software, testing (both does it function and in-situ patient testing) and compliance (to check it complies, – but not to apply for the rubber stamp unless the government works out a way to support this project). That way – crucially, we keep out deeply political or spammy non-relevant chatter. It also allows our peers to review progress in their area of expertise. Could GitHub or similar be used to manage this?
12. KEEP IT AS SIMPLE AS POSSIBLE. Simple but spec compliant. From software to parts.
With the greatest minds here coming together – engineers, project managers and skilled designers, coders, hackers, electronics and the resources of our workplaces – lab and testing and pcb design and build, etc – we could create something that the people should easily make using either manufacturing and plant capabilities – all the way down to a 3d printer at home and some electronic components.
As a signoff to this comment, think more towards the Apollo 13 moment where they have to construct something to survive out of parts they have available.
I recognise the above needs far more thought – but we need to coordinate and use as much available expertise as possible and work together quickly to make this happen. Peer review is crucial – but we don’t just want ‘Sandcastle stampers’ – please be constructive with your comments and always propose a better way with detail – if you think a suggestion is wrong.
Paul.
Just been having a bit of a brainstorm with the vent idea. The idea I had been having would be to 3d print a cylinder frame, which could then uses a thin low pressure plastic – cola bottle style. You could also 3d print a TPU Bellows running on a piston to pump air. Also thinking now about printing a TPU inline non return valve. Other thoughts i have had is that a standard Pi board with a sensor on the pressure in and out would give a good start to driving the mechanics of the pump. Add in a volume control on the pump to set the patients flow and volume.
There are a lot of options – please help fill in the lit review with the tech you know about: https://www.appropedia.org/Open_source_ventilator
Love this!
There is an open source initiative that is ALREADY being organized by this person:
Bruce “Stay Home Now” Fenton
@brucefenton
CEO Chainstone Labs, Atlantic Financial, FINRA member, veteran US Navy Corpsman, volunteer at @NECSI
Please read this tweet, which leads to a longer Medium article which tells you how to organize, contribute by calling contacts in the industry, suppliers to supply parts, pool research, evaluate ventilators, etc.
https://twitter.com/brucefenton/status/1238966762290515969
https://medium.com/@brucefenton/we-need-ventilators-we-need-you-to-help-build-them-30805e5ee2ea?source=linkShare-c89e6d55ed17-1584227433&_branch_match_id=767024742387936155
PLEASE JOIN FORCES
https://www.endcoronavirus.org/
Any chance oxygen bottles from welding could be used? They have decent regulators. Also to continue the theme, what about using positive pressure respirators from welding suppliers, such as the 3M Adflo systems, running the air through a hydration/heater aspiration rig of some sort. Do the tubes have to be medically shaped, or could sterilized accrylic hose be used. If so what diametre, what flow rate, what shape. How do we get a 3d model of the right shape to all those with 3d printers. I have seen these work down to some pretty fine tolerances… Sorry if my questions are naive.
Don’t reinvent the wheel. There are lots of tried and true simple machines off patent like the Bird Mark 7 respirator.
https://patents.google.com/?q=Bird+respirator&oq=Bird++respirator
It’s happening in Italy already.
https://www.3dprintingmedia.network/covid-19-3d-printed-valve-for-reanimation-device/
If a 3dscanning company were able to dismantle an existing ventilator and scan all of the parts, then they could be sent around the country to 3dprinting firms to duplicate. Then the electronic parts could be sourced from the nearest to spec such as pumps, psu’s etc voltage Measurements could be could be copied from the microcontroller output and pretty much copied using an Arduino with an lcd screen module and a few knobs and buttons going into and out of analogue and digital outputs. We could basically do what the Chinese have been doing for years and clone the products. Then all they would need is minor calibration adjustments.
Would this system work?
http://www.mhs.ox.ac.uk/collections/imu-search-page/record-details/?thumbnails=on&irn=16457&TitInventoryNo=10349
If we are able to get the drawing , then we can 3D print some of the parts and see how to replace it with a suitable belloe
Has anyone posted about the Hattler Catheter yet?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2002488/
Hi All,
I’m a Manufacturing Engineer / Software developer and have contacts with Semi-automated production line manufactures.
Please contact me via email if you want any information or need help designing a production process more than happy to help and share knowledge
Calum McCullough
calumjmccullough@gmail.com
Would it be possible to use automotive aircon units to deliver the required flow rate? Available all over the world.
This seems well thought out…
https://web.mit.edu/2.75/projects/DMD_2010_Al_Husseini.pdf
Andy,
Love the simple design using preexisting equiptment . It can easily be scaled up and inexpensively. Would work well for undeveloped countries where constant source of electricity is not a given. Low tech and easily understood.
steve b M.D.
HELLO EVERYBODY!
I’m following this topic with great interest, just wanted to let you know that an italian hospital as requested help to an engineer to 3D print respirators valves whom where in great need from the doctors.
Here’s the article: https://www.ilfattoquotidiano.it/2020/03/15/coronavirus-nel-bresciano-mancano-valvole-per-respiratori-ingegnere-ne-stampa-100-in-3d-coperte-da-brevetto-non-possiamo-fermarci/5737309/?fbclid=IwAR1kRwU2tQ7ERR7TuxaWEaPwpLzN_ryKGbgHyOHo5H892n8yNlK7W7E2sUY
“We no longer knew how to give oxygen to patients in sub intensive care. The valves for the respirators were finished and would not arrive in time. But the 3D printing of the pieces saved us “. To speak is Mauro Borelli, General Manager of Asst Franciacorta. In this area straddling the Brescia and Bergamo areas, there is the Chiari hospital, one of the fronts of the battle against Covid-19. For several days, supplies of valves for respirators had been exhausted and the supplier company would not have been able to satisfy the request. So through the word of mouth launched by the Giornale di Brescia, we came up with the idea of printing them in 3D thanks to the engineer Cristian Fracassi and his team. Within a few hours, the engineer replied the piece that was tested in the department: “The first tests seem to be positive, the doctor was very happy – explains Fracassi – now we cross our fingers”. 24 hours later, the signals are positive and another 100 valves were delivered to the hospital this morning: “Someone will go wild because they were pieces covered by a patent – explains the general manager Borelli – but people die here, we cannot stop. This is a war in time in peace and we must thank you for giving us these valves. ”
I’m sure this could be of great help
Best,
Daniele
Would it be easier for industry to build liquid ventilators where a fluid like perfluorochemical is used the O2/CO2 exchange?
Building basic machines for Handling, controlling and monitoring liquid flow may be easier than building gas flow devices from scratch.
No, I’m pretty sure it would be horribly complicated and incredibly susceptible to going wrong, with all the systems it would need to keep it running. Then you’d end up having to pour germ-ridden fluorocarbon out from your patient’s lungs into a bucket before they drowned.
Anyway you’ve seen The Abyss. That was meant to be a solution to diving ever deeper. Must feel horrendous if you actually do it, it would tire the lung muscles quickly having to push around heavy, dense liquid, rather than air. The scene with the mouse was actually real though, the poor little bugger really was in that liquid, panicking and wondering why he hadn’t drowned yet.
It would be horribly complicated for no real gain.
“Non-invasive ventilation via high-volume oxygen harbors the risk of aerosolization of the virus and thus an increased risk of infection for the staff working on the patient.”
Thats important!
https://jamanetwork.com/journals/jama/fullarticle/2762996
Cripes! The time has come. We’ll have to start burning herbs and painting crosses on the doors of the Infected, to isolate them til
the plague,I mean a mutated cold virus, goes away forever.Is there not a way of hacking diving equipment to supply regulated oxegen?
Could water electrolysis from a diy kit create enough oxygen to enrich the incoming air of a ventilator?
Not really. Besides, are they short of oxygen? Most hospitals I’ve been to have a huge tank out the back somewhere. A bloke in a BOC lorry comes round every so often and tops it up from his huge tank. Then there’s a system of pipes that crawls round the building, looping into every ward. One pipe carries oxygen, the other one contains vacuum. They use the vacuum with an intermediate bag mechanism, so the vacuum is only supplying negative pressure, it doesn’t actually carry any waste away.
The pipes travel past every bed, and have a tap and valve by each one, so a nurse just needs to stick an oxygen mask on you, hook you up, and there you go. Once, they decided I needed a bit more oxygen in my blood so I got a pair of tubes shooting O2 up my nose, rather than a full mask.
Anyold how. No, electrolysis is a pretty pathetic and inefficient way of getting oxygen, or hydrogen. In industry, when they want oxygen they compress it and chill it til it fractions out as a liquid. They need it as a liquid anyway so they may as well rely on that to separate it out.
I looked into this around the time of SARS and considered what a minimum possible spec mechanical ventilator might look like, that also had a low oxygen consumption. It was a “bag squeezer” controlled using common industrial pneumatic parts. Interestingly the paper published in 2010 now ceases to appear when I look up my own publication list on http://www.pubmed.com perhaps because it has the word pandemic in the title.
The UK prime minister has just today put out an open call for creative solutions to the ventilator problem. Consider that your ventilator companies may not be able to simply “ramp up production” if many of the components come from China – which, even though Shenzhen is back at work, will be flooded with orders. This may be true of products proudly Made in Britain, or indeed proudly Made in the USA. Check out the supply chains. This means your ventilator design may need to be made entirely with materials, skills and components already available in your country, possibly in a distributed manner. For example where would you acquire 20,000 pressure gauges with a range of 0 to 100cm.H2O ? This is a very low range for any industrial gauge. In the interests of speed, you may be better off creating a modern take on an old but trusted pneumatic or electro-mechanical design. In the US this might be a product by Bird for example. A VW Beetle ventilator if you like; simple, reliable, easy to fix, not for your most serious ventilated patients. Rules on FDA approval etc. and indeed vexatious medical litigation would also need to be suspended so all your staff are free to get on with their work and do their best for the patients – a wartime mentality, without having to create reams of paperwork to document everything they do. The paper I mention can be downloaded here, if I were to repeat the exercise now I would go for a different design as it would not be suitable for someone with CV, it might get people thinking though:
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2044.2009.06207.x
Thank you John for the link to your earlier design. We believe your paper has real merit and would like to explore developing a ventilator based on your paper. Therefore we are wondering what you would do differently ? Also re your alternate idea of perhaps basing a design on an old “Bird” for example do you know where we could obtain the performance and manufacturing design criteria for such a unit to consider that ? Thanks for your help.
What about this for a DIY solution?
Plastic pipe and a shampoo bottle
http://www.bbc.co.uk/news/amp/business-40498395
HOMEMADE-ventilator
https://www.dailymail.co.uk/health/article-2270178/Chinese-man-kept-alive-years-HOMEMADE-ventilator-family-squeeze-18-times-minute.html
Several years ago MIT students took on the challenge of designing a low-cost ventilator. The winning design is a contraption to compress an Ambu bag (manual bag respirator) using a simple motor and cam. This design won awards and was subsequently refined.
https://web.mit.edu/2.75/projects/DMD_2010_Al_Husseini.pdf
I think the MIT design would be a good one to use as a starting point. If the MIT design is not available, then perhaps the one from the Pandemic Ventilator Project:
https://panvent.blogspot.com/2020/03/specifications-for-pandemic-ventilator.html
I’ve read that mechanical ventilator manufacturers are ramping up production but that 50,000 units is about as much as they can do in the near term. The worldwide demand will far exceed this, so I think this project is right on track.
There is a Merck manual online that summarizes the requirements:
https://www.merckmanuals.com/professional/critical-care-medicine/respiratory-failure-and-mechanical-ventilation/overview-of-mechanical-ventilation
You have to be able to adjust the volume of air delivered, the pressure, and the interval between breaths. Too much pressure can damage the lungs of the patient (who is likely elderly and already in respiratory distress). Ideally you have an oxygen sensor, pressure sensors, backup motors and power, and alarms — but those features are probably beyond the scope of what is realistic for an effort like this. Same goes for ISO certification, patent compliance, etc. None of that is realistic for this crash effort.
What’s needed is a simple design that can push air in without too much or too little pressure & volume, a la what MIT has already come up with. And in addition to the design, we need a parts list that is readily available, and clear instructions covering assembly, testing and calibration.
Ideally, the design could rely on parts available anywhere at low cost. If automotive components such as windshield wiper motors (and their adjustable intermittent switch circuits) could be adapted into the design then you could source the primary parts from any auto wrecking yard worldwide (don’t go “Ewww!” – they’d be cleaned, and isolated fro the airstream).
It would be great if hobbyists, tinkers and self-proclaimed “Makers” could each build a handful of machines and drop them off at their local hospital. But the medical staff would require some way to demonstrate that the devices were safe and nearly as good as their medical-grade ventilators.
Perhaps a simple test device could be designed and built that could connect to each ventilator and show that it is operating well and within relatively safe parameters. There would need to be some simple way to show the volume of air delivered and the air pressure. To keep costs down, perhaps the device could be based on a simple balloon that would provide a visual gauge of performance. Observing this test device on a medical grade ventilator first, and then observing whether the test device responds similarly on the home-made ventilator, might be sufficient for the desperate scenarios we’ll soon face.
I read the MIT paper earlier today, share it with a few engineers and the it looks like ti is along the right lines. A can anyone break down what needs to be done. Ie parts list and where they can be sourced or what type of facility could make them. I would be prepared to back a project like this. Best wishes
This idea may also provide a simple way to have settable pressure and volume, it is only my notebook sketch at the moment
https://hackaday.io/project/170434-simple-ventilator-air-supply
Mike,
We have looking at the design posted by The University of Florida Health https://simulation.health.ufl.edu/technology-development/open-source-ventilator-project/. This is essentially a ventilator of last resort. The concept is to assume the presence of hospital air supply and to provide just the ventilator function. Our approach is to try to use only items found at Home Depot or Lowes and to use as little sophisticated instrumentation and control as possible. Picture manometers and reostats. Like MIT, our goal is a sub $100 unit that can be built quickly but include all of the functionality requested including operating flexibility, PEEP and anti-asphyxia features.
Word from a nurse manager friend is that FEMA has more respirators that will soon be made available to the hospitals. I have no certainty this is true, or the number involved. Does anyone have data on that?
If oxygen delivery equipment runs scarce, maybe we can round up O2 tanks normally used for welding, and round up surplus oxygen masks from airplanes that are parked in the desert being parted out because they are end of life, and connect them together. The bag in the delivery mask would minimize waste of the precious oxygen by capturing the oxygen between breaths. A single plane might yield 150 such masks, then have your local officials borrow every oxygen bottle they can. Or encourage local welders to bring their tank down for a deposit. Granted, it is not medical grade oxygen, but as a last resort it beats death.
Could valves and parts be 3d printed? Anyone willing to make a downloadable template?
Translate and read this! https://www.ilfattoquotidiano.it/2020/03/15/coronavirus-nel-bresciano-mancano-valvole-per-respiratori-ingegnere-ne-stampa-100-in-3d-coperte-da-brevetto-non-possiamo-fermarci/5737309/?fbclid=IwAR1kRwU2tQ7ERR7TuxaWEaPwpLzN_ryKGbgHyOHo5H892n8yNlK7W7E2sUY
lets all share the image of the required valve, so we can work on a good design
https://www.fabbaloo.com/blog/2020/3/16/3d-printing-helps-save-patients-during-virus-crisis-and-you-should-too?utm_source=dlvr.it&utm_medium=facebook