The number of artificial prosthetic replacement parts available for the human body is really quite impressive. From prosthetic eyes to artificial hips and knees, there are very few parts of the human body that can’t be swapped out with something that works at least as well as the original, especially given that the OEM part was probably in pretty tough shape in the first place.
But the heart has always been a weak spot in humans, in part because of the fact that it never gets to rest, and in part because all things considered, we modern humans don’t take really good care of it. And when the heart breaks down past the point where medicine or surgery can help, we’re left with far fewer alternatives than someone with a bum knee would face. The fact is that the best we can currently hope for is a mechanical heart that lets a patient live long enough to find a donor heart. But even then, tragedy must necessarily attend, and someone young and healthy must die so that someone else may live.
A permanent implantable artificial heart has long been a goal of medicine, and if recent developments in materials science and electrical engineering have anything to say about it, such a device may soon become a reality. Heart replacements may someday be as simple as hip replacements, but getting to that point requires understanding the history of mechanical hearts, and why it’s not just as simple as building a pump.
The Heartbeat of America
While the understanding of the heart as a pump stretches all the way back to the 3rd century BCE, it took nearly 1,000 more years for medical science to advance much; the early view of the Greek physician Galen that the heart provided heat for the body and blood moved from the venous to arterial systems via pores in the septum of the heart was not to be questioned, at least in Western medical traditions.
Once doctors were free to explore the human heart, its structure and function became clear. The heart is a four-chambered pump made from specialized muscle tissue. The upper chambers are referred to as the atria, feeding into larger ventricles below via one-way valves to prevent backflow. The right atrium receives deoxygenated blood from the body through a large vessel called the vena cava; it moves to the right ventricles and on toward the lungs, where through a complex process of gas exchange, it loses CO2 and gains oxygen. The oxygenated blood returns to the heart’s left atrium, and then into the powerful left ventricle, which supplies the entire body with oxygenated blood via the aorta.
Looking at the heart mechanistically, it’s easy to see why attempts at building a mechanical substitute for it extend all the way back to the 1930s. Soviet scientist Vladimir Demikhov was the first to try a mechanical heart, a device of his own design which he put into a dog. The animal lived for two hours after surgery.
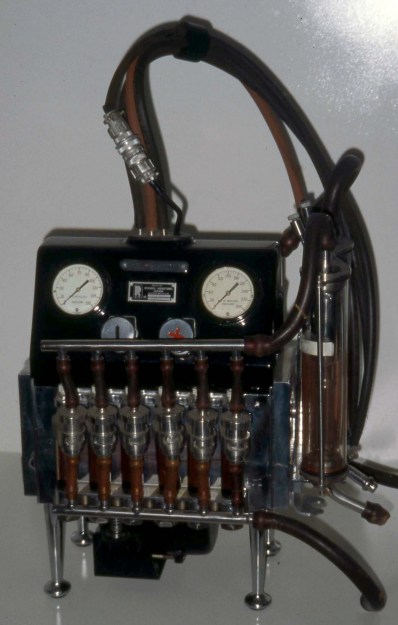
Other surgeons used Demikhov’s dog experiments as the basis for human artificial hearts, first using extracorporeal devices like the Dodrill-GMR, a device built by car manufacturer General Motors Research. The Dodrill-GMR was used in 1952 to bypass the left ventricle of a 41-year-old patient during an operation to repair his mitral valve; he survived 50 minutes on the machine and ended up living for 30 more years.
Early experience with the Dodrill-GMR and follow-on heart-lung machines gave doctors valuable feedback on what works and what doesn’t work when it comes to pumping blood. After all, blood is not a simple fluid; it’s a complicated liquid tissue that is composed of blood cells (erythrocytes and leukocytes) as well as plasma. The heart is optimized to pump this fluid, introducing as little turbulence and shear forces as possible to keep the cells intact. Any mechanical substitute for the heart must not introduce such disruptive forces, which are liable to result in injury to the patient.
A Bridge Too Far

Early efforts at mechanical circulation focused on completely extracorporeal devices, acknowledging the fact that the engineering of the day was nowhere near ready to provide a totally implantable artificial heart. But the dream of a mechanical replacement heart lived on, mainly because the demand for healthy human hearts for transplant continued to outstrip supply. This became more and more the case as engineering for motor vehicles improved through the decades; the sad fact is that auto accidents provide the most reliable source of viable donor hearts, and as cars got safer, the donor pool got smaller.
The first so-called total artificial heart (TAH) to capture widespread attention was the Jarvik-7 heart, which was used for the first time clinically on Barney Clark, a retired dentist with severe congestive heart failure. Despite the fact that Clark had to be tethered to a large air compressor for the 112 days that he lived after surgery, the Jarvik-7 was the first artificial heart where the pumping mechanism was completely inside the chest cavity. It set the standard for what counts as a total artificial heart even today — the pumping mechanism is implantable, but due to engineering limitations, they have to be powered from outside the body.

Both of the total artificial hearts currently approved for use in patients today rely on external power. The SynCardia TAH, a direct descendant of the Jarvik-7 heart made with better, more durable materials and equipped with valves that are less likely to damage blood cells, is still powered by compressed air, although the drive unit has been miniaturized enough that patients can go home with one. The other TAH, made by French company Carmat, uses a hydraulically driven flexible diaphragm to pump blood. The hydraulic power pack is small enough to be carried around, and is powered by Lithium-ion batteries.
Despite their mechanical differences, both these devices have something in common: they are not intended to be used as permanent replacement hearts, but rather as a bridge to buy some time for a donor heart to become available. The main reason for this is simple material science: it’s very hard to find materials that can flex continuously 70 to 80 times a minute for years on end without tearing. The best Carmat has managed to do is about 1,400 days, and while that’s more than ten times better than Barney Clark’s experience, it’s nowhere near enough. The other problem is that routing pneumatic or hydraulic lines into the thoracic cavity is clinically problematic, primarily through the risk of infection.
No Pulse, No Problem
While it might sound like a permanent TAH is still a long way off, there’s a lot going on in this space that might shorten the journey. A startup called BiVACOR is working on a design that’s vastly different than the SynCardia or Carmat hearts, and it contains components that will look very familiar to any hardware hacker. Rather than rely on diaphragms to move blood, the BiVACOR TAH used a centrifugal pump, whose impeller blades are directly in contact with the blood and provide a continuous flow. Normally, this would be an unacceptable source of shearing forces that would tear blood cells apart, not to mention the need for bearings which would eventually wear out. The BiVACOR TAH avoids these issues by magnetically levitating the impeller, leaving a wide gap between it and the pump housing. The gap distance is monitored and adjusted continuously so there’s no mechanical wear and no shear forces on the blood. The double-sided impeller is the single moving part in the pump, and is driven by what looks very much like the stator coils of a brushless DC motor.
One of the big advantages of the BiVACOR TAH is that it’s far smaller than the current crop of TAHs. That’s important because the space available in the thoracic cavity is quite limited, even in large male patients. Female patients and children, who tend to have smaller hearts, are often difficult to fit with a TAH. The BiVACOR heart also ticks the box of less intrusive external power; electrical cables are much easier to route into the chest cavity and less likely to act as a conduit for infection. It’s also quite possible that advances in battery technology will make implantable power sources possible in the near future; coupled with transdermal inductive charging, the BiVACOR heart and those like it could be the first practical permanent total artificial hearts.
There’s clearly more to do here; some basic questions, like does the human body have a physiological reason for a pulse, remain to be answered. Luckily, the BiVACOR heart can be programmed to provide pulsatile flow, so they’re well-positioned no matter what the answer is. But the fact that we don’t even know the answer yet shows how far we have to go. Luckily, the engineering appears to be catching up to where it needs to be for a permanent artificial heart to finally become a reality.

















“there are very few parts of the human body that can’t be swapped out with something that works at least as well as the original”
Huh? Is this serious?
Prosthetic eyes? You mean glass eyes with which you cannot see? Yeah, works like the original. Replacement lungs? Kidneys? Liver? Intestine? Muscles? Brain? Where are they?
Maybe the brain is next to the “Bum Knee”? If you have a knee in your bum then you have some serious problems….
Although the writer was engaging n hyperbole, or even ought-right falsehood, with that “few parts” bit, eyes _are_ on the list. Retinal implants are currently possible and, while not great, are only implanted when they’d be better than nothing. That’s the writer’s loophole: they aren’t comparing the replacements to the parts of a healthy individual, the comparison is to the damaged or worn-out part that is being replaced.
A classmate sneezed his glass eye out in 3rd grade. You can’t do that with normal one…
I have a friend with a glass eye. He was once in a bar with another mutual friend who made the mistake of asking him “hey, can you keep an eye on my beer?” What happened next probably goes without saying, but it did involve a fair amount of shouting.
lungs and kidneys we can do, just not with a compact implantable machine.
Don’t worry about the brain, in most people it can be completely nonfunctional and it doesn’t impact their lifestyle at all, tik tok users are a perfect example.
+1
We grow meat in a lab, I’ve eaten a lab-grown hamburger. It tasted like meat. So we will grow specialized organs in a lab for people that are in need of replacement organs. It’s just a matter of time and acceptability.
Hello Me, I was just saying that there are biological fixes rather than mechanical ones, in regard to the HEART. That’s a specialized tissue unit that can’t really be replaced for too long. We will be able to grow a heart in a lab within 5 to 10 years.
I suspect the sentiment was more along the lines of “if there is a replacement, then it’s at least as good as the origional.” ie we can’t really replace a kidney, but the artificial knees we have are as good as a regular knee.
“does the human body have a physiological reason for a pulse”
That’s an interesting question, and one I’m surprised wasn’t answered already. I found a few articles from 2009 suggesting that it’s not essential (as was previously thought), eg https://www.ahajournals.org/doi/10.1161/circulationaha.108.814863. Nothing conclusive though.
Well, the movie “Repo Man” (the 2010 version) is placed in near future – 2025…
Quite a bit of work had been done on organic 3D printing of muscle tissue. Delamination and improper placement (or absent) of signaling proteins along where a basement membrane should be- are a couple non starters for creating functional replacement organs. I do look forward to the advancement of stem cell seeding in “ghost” tissue as both of the previously described problems are resolved, in this technique.
Is there a yamaha sports model with an extended warranty?
https://www.youtube.com/watch?v=ars458hcETE
Technically, I think they all come with a lifetime warranty. The length of that lifetime is another question entirely…
That’s true. My kidney is good for life, and after a partial failure two years ago, it likely will define my lifespan.
What is he saying after “Extended warranty”?
Apparently, just “Financing”. It comes through more clearly in other recordings.
It will be interesting to see what happens some day (though maybe beyond our lifetimes) when artificial organs become more reliable than the originals.
Don’t think that is possible? Consider this. Even if an individual artificial organ is never as reliable as the original, if you can miniaturize them enough to fit two in the space of one you can have a backup. Then so long as both don’t fail back to back faster than you can get to the operating table there is always a way to save you.
Normally we only think about replacing worn out organs with known problems. People don’t usually just keel over with no warning. But it does happen. Sometimes hearts just stop unexpectedly and in that circumstance it’s unlikely you will get to the hospital and get a new part swapped in before brain death.
It might make sense as sort of a coming of age ritual that everyone goes through in the distant future. Reach adulthood, (when your body stops growing) swap out your organs for bionics. There will be so much resistance to that! It’s not natural, cutting open a healthy person violates the hippocratic oath, it somehow makes you a machine and takes your humanity away… blah blah blah bs bs bs. (Obviously I am not talking about the brain)
I have a couple relatives who would be alive today if they could have done that but aren’t because surprise… heart just stopped, no warning.
I think that level of body alteration by choice is a very long way from being acceptable to society at large, even minor body mods get funny looks and such… So I would think way beyond our lifetimes, even if the tech really gets there sooner.
It’s an interesting idea, but I doubt artificial parts for the meat space really living parts of the body will ever really work long term – they will all be rejected in the end…
If you can fix that problem sticking with organically functional parts with genetic tweaking to make donors compatible across species or perhaps growing/cloning seem much more likely anyway. No mechanical system lasts forever, and when it breaks its surgery to fix, but your ‘artificial’ meat should heal itself and replace itself over time anyway, being good for a very long time and self maintaining..
All those out of the blue failures are likely a thing of the past if you can figure out how to really control the immune system to properly prevent rejection with no other issues then you probably know enough about how every part in the body functions to spot the tiniest of early warning signs and be sure your replacement parts of perfect…
But if you are sticking with organic functions there wouldn’t really be space to duplicate them all, maybe the heart can have an extra squeezed in – loose a little intestine and stomach perhaps, while making hearts that are a touch smaller than natural (if you are doing all those replacements anyway making a heart that has to beat a little faster all the time when running solo isn’t going to be the end of the world). But no way you can have backups for all the functional parts that will kill you quick when they fail – as that is nearly every organ, its just too much duplication to fit functional sized duplicates and all the extra plumbing to plug them in.
“If you can fix that problem sticking with organically functional parts with genetic tweaking to make donors compatible across species or perhaps growing/cloning seem much more likely anyway. ”
I mean, just get good at growing new organs. It’s not like your heart *actually* lasts for 70+ years – your body’s just continually rebuilding it, at a rate of around “new heart every 3 years.” Problem is that it’s doing it in place and crap and errors build up. So find a way to *not* do it in place and do better error correction.
“I think that level of body alteration by choice is a very long way from being acceptable to society at large,”
No way. If you could replace organs with artificial ones that are known to perform better and last longer then the people that could afford them would get them. Nobody is going to even notice since, you know, they are internal organs.
The real game changer is going to be when the machines we start making are actually just sythetic cells that we’ve programmed. It’s at that point where man and machine will begin to merge in any meaningful way.
The making it legal – which requires acceptance of society, is entirely different to just getting negative social interactions when such things are hidden by clothes etc… In the same way for many folks being gay, cross dressing and gender swapping still isn’t acceptable – it should make no difference to them, they probably wouldn’t actually know but its still not ‘right’ so takes ages to be legally allowed.
And woe unto you if you get caught being deviant in ways not acceptable to society at large, nice little media circus ruining your life at best… Heck doesn’t even take proof of any ‘wrong’ doing, just the suggestion can be enough to start the witch hunt.
I dunno – I think of long-term heart failure in someone with a “normal” heart (as in, no congenital defects) as more a symptom than a cause. As in, the heart fails because it’s had to work too hard due to blockages in the circulatory system (or overall heavier load). In that case, “swapping in” a heart just shifts the problem – now you might not die of a heart attack, you’d die of a stroke or other organ failure.
I kinda don’t think the *intrinsic* aging problems (cancer, arthritis, etc.) are really fixable with “better organs” – those are more of a distributed general failure issue. You’re not going to be able to replace someone’s entire circulatory or joint systems.
I seem to remember an old article about a women with two turbine based battery powered (TAH) answering the the Whole if the heartbeat was necessary. The title of the article was something the Women with no heartbeat. The Point was the unit she used was a continual flow type. So she had no pulsed heart beat. If fact if i remember correctly it had some ethical questions do to the fact that she experienced more energy for longer than usual do to the continual flow vs the pulse. But had some side effect of exhausting the batteries pretty fast under high loads. Wish i could find that article.
but here’s a link to the same device before it was used in the lady:https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiEn8y72aTyAhW3GFkFHV0fDFgQFnoECAYQAw&url=https%3A%2F%2Fwww.npr.org%2F2011%2F06%2F13%2F137029208%2Fheart-with-no-beat-offers-hope-of-new-lease-on-life&usg=AOvVaw1y–OSJfD2sQ_uhTGZSmcO
While I’ll look on developments with interesting I still believe replacement hearts will be biological (animal, lab grown, cloned, 3D printed). You fix steel with steel, wood with wood and meat with meat.
I want to become a full-body cyborg but I guess becoming a bioroid is acceptable, too.
The reason why we have a pulse might be that the heart works at “only” 1-2 Watts. Pretty nice overall efficiency I’d say
“Whew, my heart rate is up to 600 RPM!”
“. . . You mean 60 BPM?”
“No.”
Figure out how to grow a biocompatible electric organ based on what the electric eel has, but regulated to generate a continuous stream of electrical pulses. Implant in the abdomen to power a heart pump. Ideal location would be in place of a failed kidney.
Why not just have a charging session while on dialysis?
Three times a week, five hours each
One thing I didn’t see mentioned (maybe I missed it) was how the artificial heart would be regulated (sped up/slowed down) according to workloads required by the body. Having a heart pumping at one flow rate would preclude many activities. (In Space 1999 Dr. Bergman had a wrist device where he controlled his artificial heart)
Maybe it will have a built in oximetry, at normal levels keep a steady volume flow, O2 goes down increase the flow?
This article compared with the recent article about future airliner designs beings up an interesting juxtaposition.
Airliners keep people alive with lots of redundancy. When there is no redundancy, the planes crash (as in 787 max).
But the human body has very little redundancy. Lots of single points of failure. And we generally last a pretty long time.
Nature is smart. Maybe we should revive the art of making things never break (like the old lightbulb in the fire station).
737 max.
“But the human body has very little redundancy. Lots of single points of failure. And we generally last a pretty long time.”
Uh. No. The human body has *ridiculous* redundancy. The human heart isn’t a “thing” like a pump. It’s actually millions of cells. And *tons* of those cells are perfectly capable of rebuilding huge fractions of the entire heart in weeks.
Saying that the human body has very little redundancy would be like saying that a swarm of bees has no redundancy because they’re just one swarm, or an ant colony has no redundancy because it’s just one colony.
“Nature is smart. Maybe we should revive the art of making things never break”
The human body breaks *all the time*! Cells screw up replication often. You know what happens? They say “oops” and off themselves, because *one cell* isn’t important at all, and there are millions of others that can take their place.
I work in this industry, have designed a few LVADs and TAHs, I’m happy to answer any questions anyone has.
Great great.. will someone PLEASE make acceptable artificial spinal discs and meniscus for knees?! Come on people!
lol
I like how there computer model showing the waveform ends in a long flatline.
Brutal.
If the FDA still can’t approve the Pfizer-Biontech SARS-CoV-2 Alpha vaccine, they are never going to approve an artificial heart. At least not unless the heart’s approval can politically benefit one party over another.
Actually, they already have (approved an artificial heart) https://syncardia.com/patients/home/
I actually know a person in long term study of artificial heart now. Been in it several years. Has a “fishing vest” he has on all the time with battery packs in it.
“Permanent Artificial Hearts” are already here—simple don’t replace them and they become the last one someone will ever need.