Sometimes we dig through the archives to see what kind of crazy hacks we can pull out of the depths of the world wide web and this one was worth sharing. Researchers at Northwestern University developed a sticker that’s applied to the fingernail and measures heart rate, motion, and blood oxygen, all without a battery.
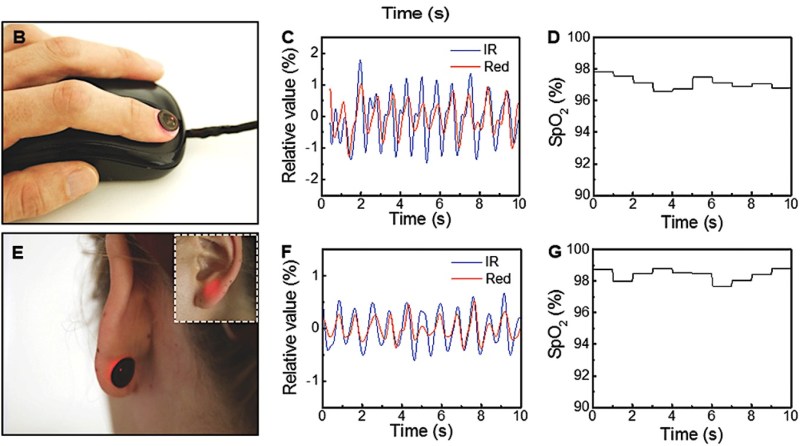
The photoplethysmograph (PPG) system is similar to what we’ve covered before and the motion sensor is simply an accelerometer, so we won’t go over those aspects of the device. The parts of the device that did catch our attention were the battery-less operation as well as its size. It’s just so dang small! And fits snuggly on a fingernail or on even on your earlobe. The size here is actually a very interesting feature and not just a marketing plug. Because the device is so small and lightweight, it is very easy to adhere to the fingernail or skin with very little sensory perception. Basically, the person wearing the device won’t even notice it’s there. That’s definitely an advantage over the traditional, bulky, hospital-grade instruments we’ve grown accustomed to.
The device adheres really well given its small and lightweight design, so motion artifacts are significantly reduced. Motion artifacts in PPG-based devices are due to the relative motion between the optode (LED and photodiode) and the skin. The traditional approaches of ensuring the device don’t move are for the patient to keep very still during a recording, to wear the device tightly against the skin (think of how tightly you need to wear your smartwatch to get consistent readings), or use some seriously tough and uncomfortable adhesive as you may have done if you’ve ever gotten an electrocardiogram reading before. This device eliminates those three problems.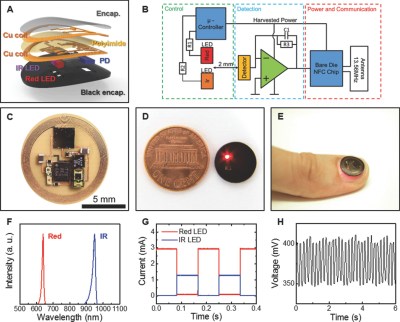
The other aspect of the device that caught our attention is its use of wireless power instead of a battery. In some senses, this could be seen as an advantage or as a disadvantage. The device relies on NFC for power and data transmission, a pretty common approach for devices that only need to be used intermittently. Wireless power could be a bit problematic for continuous monitoring devices which provide readings every second or several times a second. But who knows, wireless power seems to be everywhere these days.
Digging into the details a bit, the double-layer antenna is designed around the circumference of the device using wet etching to create traces on a copper polyimide foil. The team electroplated holes through the different layers of the device (optode layer, first antenna layer, polyimide, second antenna layer, component layer, protective top coat) connecting the antenna to the die pad NFC chip (SL13A, AMS AG). Connecting the chip requires some pretty fine-pitch soldering techniques, but nothing we’re not accustomed to here at Hackaday. Overall, they seemed pretty successful, obtaining a Q factor of 16 and a transmission distance of 30 mm using a smartphone and not some giant reader antenna.
Definitely, a really cool project that we recommend checking out.













Flooding a hospital room with a 13.56 MHz signal seems problematic considering they do everything to avoid RF emissions. However, I think this would be great for hospice care or at home care.
They avoid /uncontrolled/ RF emissions. There are plenty of RF devices in use, and avoiding interference with /those/ is why the emission control measures are in place to start with.
Oh man. So close to an implant. I think question is when, not if.
I’m surprised the didn’t power it via the thermoelectric effect. The difference between body temperature and the ambient environment. A thin slither of aerogel or similar. I can’t help but imagine the spy technology equivalent.
I’m not surprised, because that would be a terrible power source. You’re got at most around 1 cm^2 of area available, and a temperature difference of around 13-17°C (assuming 20°C room temperature and normal skin range of 33-37°C). That gives you around 1.4 microwatts of power (https://ieeexplore.ieee.org/document/9629473). Their Q=16 coil and 4W transmitter gives them probably around a 10% efficiency, or 400mW available power, or nearly 300,000x what would be available from skin thermal gradient power.
These devices, just like the current pulse oximeters, will suffer from low blood pressure situations. When someone is hypotensive the physisological response is to conserve the brain, heart and lungs; peripheral circulation shuts down to shunt to the critical organs. Fingernail beds and earlobes work well as long as blood pressure is decent and temperature are in a normal range. On the floor, not the ICU, I can see some potential benefit, but the majority of patients on the floor are not continuously monitored, that level of care generally occurs in units handling more acute patients.
I’m not criticising the work, just pointing out that the fundamental physiology remains a critical factor. As to the adhesive, in my 10 years in the ICU, there were virually no adesives that worked “well” in all, or even most cases, not to mention allergic reactions to many adhesives.
The reference to electrocardiograms requiring little to no movement for the recording is actually not relevant to pulse oximeters recording data. ECGs respond to electrical activity in the muscles, so movement adds tremendous levels of noise (in the ICU it’s not uncommon for heart monitors to alert to fatal rhythms when someone is brushing their teeth, rolling over, etc.). The number of machines alarming in the ICU can lead to level “alarm deafness” in RNs and MDs since they are going off repeatedly. On of the aphorisms in hospitals is “Treat the patient, not the monitor.” That is, go LOOK at your patient to see how they are.
Final thought is that the continuing search for any approach that reduces patient discomfort while monitoring is a laudable goal, and one that I do encourage.
I usually notice when I stop breathing. Well maybe not four years ago, when they said I had an oxygen mask.
Being blue on the lips or even dead usually is a good indicator… And, it’s free