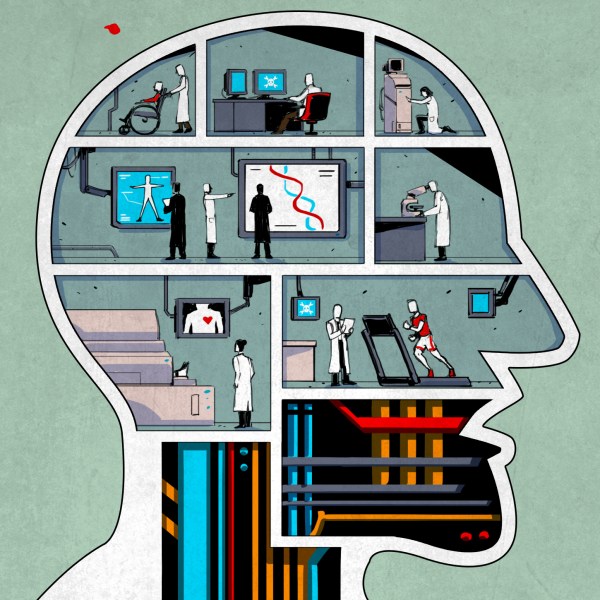
Although there are many skilled and dedicated types of health care professionals, nurses are often the main point of contact between the medical establishment and a patient. You will probably spend more time with your nurse–especially in a hospital setting–than any other health care provider. Every patient’s needs are different, so it isn’t surprising that nurses sometimes improvise unique solutions to help their patients be more comfortable or recover faster.
That’s the idea guiding an innovative program called MakerNurse–an initiative backed by MIT and the Robert W. Johnson Foundation. The idea is to encourage nurses to be makers. One of the project’s cofounders, Anna Young, had found nurses in Central America making do with what they had on hand and naturally acting as makers. “We saw a nurse repair a stethoscope diaphragm with an overhead transparency,” she said. Young noted that often nurses didn’t realize the significance of their making–it was just how they got through the day.
With the MakerNurse program, Young’s group surveyed nurses across the United States and then went to five hospitals to study what nurses were making and what support would help them do even more. The study, which will be published next year, identified resourceful maker projects from nurses and even collaborations between nurses, patients, and their family caregivers. One gadget found in Massachusetts made it easier to feed a patient with a feeding tube. Young said, “It was simple, it was sturdy, and it solved a very clear problem.” It was made with material the patient and their family bought at Home Depot.
The logical conclusion: makerspaces in hospitals. Young has made it happen, and the University of Texas Medical Branch’s (UTMB) John Sealy Hospital in Galveston Texas has the first of what she hopes will be many such spaces. The UTMB MakerHealth program provides a permanent facility for nurses (and others) to build custom solutions to make their jobs and patient’s lives easier. Users can receive training and other assistance to take their ideas to reality.
I asked Young about the ramifications of making what amounts to medical devices. She replied, “Hospitals already have the processes in place to do investigational studies, and these are treated just like those studies.” She also mentioned that they ensure that appropriate materials are available for the makers. Her belief is that these makerspaces will enable nurses and others to do work that wouldn’t have the volume to warrant a large study (like the left handed arm board for cardiac patients seen in the picture above). In addition, the facilities will allow “one off” pieces (like a custom cut bandage) to be easily and precisely replicated.
An MIT spin off, Pop Up Labs, provides logistical support and training for the initiative. The makerspace will have a dedicated manager and soon will also have a “Maker in Residence” to help with designs and builds. Young says that many nurses are “modest” and need encouragement to bring their ideas forward and things like hackathons and mobile maker spaces tend to miss less vocal potential makers. The MakerHealth web site is an online community Young hopes will “bring the sharing of the Maker movement into healthcare,” and encourage more health care creations.
The videos below show more about MakerHealth, including a tour of the facility. We’ve already seen hackers make big impacts in STEM education and thanks to these initiatives, the hacker culture may start having a similar effect on hospital patients. The pioneers of the Internet probably couldn’t imagine how the net would revolutionize our world. Likewise, it is hard to know just where our culture with its emphasis on creativity, openness, and sharing will lead over time as it continues to spread beyond our traditional community. I’m excited to see where we’ll go next as hacking and making filter into the mainstream.












As the husband of an ingenious nurse, I thank you for this article.
This may be just the ticket to get her to buy-in on a 3D printerer!
When one of my daughters started nursing school (she’s a NP now) I bought her a red crayon. I told her it was in case she had to draw blood.
LOL!
Cross pollination between disciplines and problem spaces is very useful. The number of little islands of domain specific knowledge and human ingenuity applied to what look like domain specific problems but which may be just individual instances of general problems make it well worth looking to other disciplines and problem spaces for inspiration when considering a touch problem in your own domain. There is a surprisingly good chance that a nurse, plumber, lab tech, process control engineer, etc… (Any hands on problem solving profession really) has solved a similar problem in a different domain such that it can be translated to your problem space.
Hey MIT and MakerNurse, have I got an Idea for you:
I think that you should develop a modular, self-triage unit for emergency room use.
Think about all the times you, or some you love, has had to sit in the ER for hours being exposed to diseases like Influenza and MRSA because of the intake and triage bottleneck.
Think about how a large number of these patients are capable of entering their personal information and running simple diagnostics, like taking their temperature, blood pressure, SPO2, or wound photos themselves.
Think about how the current technology heavy environment is fostering an entire generation that would rather interact with a device than a real person.
Now, consider the benefits of such a solution. The line at the intake desk is much shorter, the triage nurse is better able to prioritize the patient load, and throughput to the actual ER can be increased.
Best of all, this can be accomplished with existing hardware/software.
Why not give it a try?
Four words: “Liability” and “Patient Safety” and “Cost.” To take the simplest of examples: If a patient takes their own vitals, a healthcare provider has to do it over simply to ensure that the data is correctly attained. A decision made because the data is incorrect may have lethal consequences. That hits the patient safety and liability. Beyond that, the time to take vitals are generally so small of time that the cost of having all the extra equipment available for each potential patient is prohibitive compared to the cost saved in provider-hours. Lastly, and this is the decision for which the legal department will say absolutely no to, who is liable if a patient takes their vitals and then crashes?
The purpose of the triage nurse is to stratify and properly divert the potential patients so that the most critical patient(s), and soon-to-be critical patient(s) don’t decompensate in the waiting room- NOT so that everyone can be seen as quickly as possible. Its unfortunate that the ER is considered the de facto place for health care, but if only critical patients came to the ER and everyone else went to a primary care provider like they are supposed to- a big portion of the dilemma to providing quality healthcare would instantly be solved. Oh, and the patients would be seen faster with the existing hardware/software.
Never heard that word “decompensate” before, nice word! The step before “decompose” I suppose.
“Its unfortunate that the ER is considered the de facto place for health care…”
Agreed. But, since it isn’t likely to change, shouldn’t something be done to remedy the issue?
Second, where liability and safety are concerned, I am not suggesting that the patients who have merit to be in the ER should be sent to one of these kiosks. Rather, I could see the person with a few stitch boo-boo, or the the sniffles making use of it.
Regardless, after my first cardiac issue and during my second, I was forced to wait in a two-hour holding pattern because the receptionist thought I was faking because I was ‘too young’ for such a complication. If I had been able to step into one of these kiosks, any doubt would have quickly subsided.
In fact, the only reason I was finally seen was because one of their passing social workers clearly understood the liability they would have if I had died after waiting that long behind patients with the sniffles. So, liability and risk exists either way.
Finally, I understand why the triage nurses are there. But, I think this could be an effective tool for them to help ameliorate the burdensome use of the ER.
It’s the same story that you see quite often in “Maker” stories with medical devices.
We made a medical device that is a fraction of the cost of existing medical devices on the market! And all we had to do was skip all the FDA approval and other regulation, quality control, insurance, manufacturability, testing, confirmation of safety and efficiacy etc that apply to medical devices!
Something that plugs in a mobile phone might be good for this, saves on power supply, display, interface etc. Have a QR code or whatever, maybe a local Wifi network that leads just to a homepage for the app. The app leads you through where to put the probes, which can be colour coded. You could even do EKG, the pads are disposable anyway.
A patient’s friend, or maybe a volunteer helper, could help the person attach the probes etc.
Still, there might be problems with patient acceptance. And I dunno exactly how useful SpO2 or mmHg would be, as it might well be that a patient who has serious problems with those would look sick enough just on appearance that a nurse would know to elevate their priority. And certainly those measurements would need to be taken again when the patient is attended to, you wouldn’t want to rely on them when medical staff are available to do them again properly.
Suppose like most things, depends on price and usefulness.
On the subject, I can see in the sue-happy USA, patients taking the opportunity to sue if non-standard, non-approved equipment was used on them. Even if it was better than the standard stuff. Hospitals have to be conservative about that, sometimes to the detriment of patients’ health, but you can’t really blame them. Approving medical devices now costs a ton of money, and needs experts with big labs and studies. Might be useful for poorer countries though, where medicine and money aren’t so closely tied.
I wish it could be this easy, but the FDA, AMA, and all the other bodies of governance an wouldn’t allow a BYOD solution; because that would incorporate too much risk.
Regarding the diagnostics mention, it could have given them nearly two extra hours to lessen the damage to my cardiac tissue. My BP and Pulse were so obviously out-of-bounds that upon receiving them, the RN would have known that I had a legitimate issue.
As a physician and a maker, I applaud the effort. But there are some serious challenges to this concept being taken mainstream: hospital contracts usually have an IP clause in them that state anything a health care provider invents becomes property of the institution without any tangible reward; AND these creations do not generally allow for fast track approval through the Food and Drug Administration, nor recognized practice of any state medical board.
To be clear, the ramifications are that there are no financial rewards for going above and beyond what you are credentialed for, but you will take on MASSIVE liability if a “made” creation finds its way to being used on a patient without being tested thoroughly for safety and efficacy- let alone the circumvention of the IRB board for the hospital, leading to a possible termination. For these reasons, this concept works- and has been working- in countries/jurisdictions that do not have these safety-minded and legally-binding protocols in place.
Now, maybe some nurses don’t worry about losing their license or being sued into eternal poverty status. But having survived a malpractice suit -just the risk of it, for something as polyannic as this, with absolutely no legal protections- no thank you.
I asked Anna Young about this and (as I mentioned) she told me this all gets done through the hospital’s existing “investigational studies” — so I think they’ve thought about this although I’m not expert enough on the legal side or the FDA side to tell you if I agree with their posture on it or not. However, this wasn’t just a few workers throwing together a space, so if I had to bet, I’d bet they have the angles covered. I’ve indirectly seen what FDA approval looks like so that question was on my mind too.
Not to mention if a Nurse were to fix a stethoscope, there’s no guarantee that they would’ve fixed it well, and it might subsequently be used to fail to detect a heart problem which could lead to death.
I’m should hope that most hospitals only allow bodged/hacked equipment to be used under extremely strenuous circumstances, but then again I’m not too sure about the state of American medical care…
If it’s say, the lamp above a patient’s bed, then sure. But equipment used for diagnosis or treatment? Nah.
That’s Al for clarifying.
Thank you clintleclair for your concern here! So much to add and so much to be careful about.
Let us try to clarify.
It’s not Make —> Stick-into-patient
It’s about Idea–>Make–>Test—>Lots of Ethics Gates—>Test—>Eventually FDA approval
No one in any hospital we are associated with is circumventing any ethical protocols. We don’t do that at MIT where our approaches were born, we don’t do that in field where they grow and we don’t do that with our HealthSpaces.
Medicine is the only field where the medical industrial complex can easily squash and scare upstarts and new ideas by telling people: you shouldn’t do that, you might hurt someone.
There’s many pathways to diffuse devices and we are helping our hospital with these.
Generally this is only the word of a biomedical company watching over the nurses and doctors to see where they spot some opportunities to develop their products. Nurses, doctors and patients deserve a better seat at the prototyping table. Our approach enables that.
IP: Of course, any employer will have a share of what you invent. At MIT where our roots are it’s roughly 40/60 (inventor/MIT). We have seen this is generally the same at other institutions and that’s a fair split considering they are fronting the cost of infrastructure and legal fees.
This is making though and as Hackaday readers will appreciate. It’s just about patenting. It’s democratizing the fabrication so more people can generate these solutions.
Sorry for the above typo in the last paragraph.
Correction: This is making though and as Hackaday readers will appreciate. It’s NOT just about patenting. It’s democratizing the fabrication so more people can generate these solutions.
If it is true that it’s not just about patenting and more about democratizing the process, then universities and hospitals would not have the intellectual property policies that they do. Unfortunately, these policies sabotage the very innovation that makerspaces claim to encourage, because they are less about democratizing/empowering and more about taking and profiting from other people’s ideas. For the universities and hospitals that finally realize this and use their lawyers to support and protect inventors rather than institutional interests, what they will find is that they will receive much greater financial return from free will gifts of successful entrepreneurs who they fostered, and when word gets out on their innovative, truly democratizing policies, talented visionary innovators will flock to their institutions and skyrocket their reputation and ratings.
This is fundamentally needed in every angle of medicine. I do not understand why that 3D printed cast + ultrasonic transducers to speed up healing of bones was not replicated by hacker spaces immediately.
I hope something like this starts in PDX. I’d love to know if anyone here has a 3D Printer I could supply the materials for to experiment with offering this service for free.
Cara…actually we’ve been trying to do this. Navigating hospital policies and procedures is a long process…
I totally get that 3D printing an artificial heart or a surgical tool wouldn’t fly. And a self-triage kiosk might have the wrong risk profile for an ER. But look at the examples in the videos: a leftie arm board, a custom tool belt, a special-purpose shower head system, a kid-resistant IV cover, a specially cut bandage. These are BASIC, MODEST innovations that can help nurses take better care of patients.
Maybe instead of immediately calling the legal department, wait and see what kinds of things these experienced practitioners come up with.
Maybe you are right regarding the risk profile.
Could still build it and put one in every mall in the country, touting them as “Checkup Kiosks” and putting a big fat disclaimer sticker and splash screens indicating that: ” The information provided by this kiosk does not constitute medical advice. If this is an emergency, please exit the kiosk and dial 911. “
Whoops, forgot my bill acceptor and magstripe reader… Gotta get paid.
Is it that hard to take your own temperature, blood pressure and sugar at home? What would you incorporate into these kiosks to make them special?
I am an OR nurse in a level one trauma center. There is a big difference in “expertise” when it comes to ER/TRIAGE nurses in a hospital that is not level one. That said, there are great nurses and not so great nurses in both facilities. Nothing beats a hands on assessment. I can tell more about a patient by looking and talking to them than my equipment can and a heck of lot quicker. As had been stated above, the liability keeps most people in the medical industry from wanting to invent and then the lack of compensation also tops the list of why ideas do not get out. In an industry that I will get sued if I tell a patient “everything will be ok” does not cultivate innovation.
Mom was a nurse…(before employment at as a QA at a solid rocket booster company…) She abhors current standards inside the current medical practices standards.
What I have been able to extrapolate from her experiences and based on current standards…
I understand in some locations doctors have voiced their objections in order prevent lack of common sense to cause problems.
1.) Footwear – How often do people wash their shoes? Not often… worse yet Crocs.
2.) Fake nails – How well can you wash between the fake nail and real nail?
Bacteria. How do they work?
http://bacteriality.com/2008/05/biofilm/
http://www.uchospitals.edu/news/2009/20091125-protein-armor.html
http://news.softpedia.com/news/Bacteria-Species-Can-Build-Radiation-Shield-155830.shtml
more legit?
http://onlinelibrary.wiley.com/doi/10.1002/jbm.820250706/abstract;jsessionid=603D65284AD776E1D2BEF865B46EB29D.f03t02
http://www.ijaaonline.com/article/S0924-8579%2810%2900009-9/abstract
Unless it is has Iodine or Chlorine that shitty Jar of hand sanitizer just gives everyone a false sense of security.
3.) UV proof contact lenses and SPF 100+ should be standard issue.
4.) No personal autoclave stations or thresholds to filing office.
5.) No raw UV lights in the A/C and Heating duct work.
6.) Door-handles, scales and pretty much everything that is handled and metallic should be SILVER electroplated.
7.) Clerical workers with little or no medical training handle the same workstations, pens, paperwork as nurses and patients.
A.) Nurses, Nurse assistants and Orderlies suffer a great deal of stress and suffering attempting to connect with patients because they are FORCED to use empathy. Convalescent, Urgent Care and Hospice workers – should have free available counseling and mandatory 6 month sit downs to gauge how much empathy they expending (pull back the feels) OR conversely how much apathy they have (it’s all just walking talking meat). Much of the time they can only rely on each other or family for resolving feelings of grief.
In the most foolish analogy I can conjure; Even a dove can turn into a bat with enough neglect surrounded by other bats.
Hey Nurse Makers: Make me some Affordable health care pleeze.
A suggestion: stop using the word “maker” and “making” and use “3d printing.” It’s confusing readers and makes you guys sound more hip rather than help you communicate anything meaningful.
Well in this case I think it was the better word because if you look at their setup it isn’t just 3D printing. It is a lot of different tools. For example, they were showing bandages being cut using some cutting tool and people creating items using more conventional tools. So while I often agree with you, in this case I think “make” or “create” or something was really the right word. The 3D printing was just one tool they provide.
Thanks for clarifying Al. Absolutely, it’s a lot more than just 3-D printing. In fact, we learned so much from nurses to make sure the right tools are in the right place. We all have our favorite gadgets. 3-D printers are fun, but there’s sooooo much more. I mean something as simple as Sugru and colostomy glue can do wonders! :)
Drone, we have affordable on-demand healthcare at TeleNurse Network.
Open Source. Read up on FOSS.
Proprietary can kill you.
Government should not-prohibit limited liability healthcare. Someone could open a hospital, use non-FDA approved stuff, be able use unlicensed staffed, and be protected from frivolous lawsuits.
Then those who can’t afford the over regulated healthcare, can use it. It could also be a place for innovation.