The Glia project aims to create a suite of free and open-source medical equipment that can be assembled cheaply and easily when and where it’s needed. Even essential tools like stethoscopes and tourniquets can be difficult to acquire in certain parts of the world, especially during times of war or civil unrest. But armed with a 3D printer and the team’s open-source designs, an ad-hoc factory can start producing these lifesaving tools anywhere on the planet.
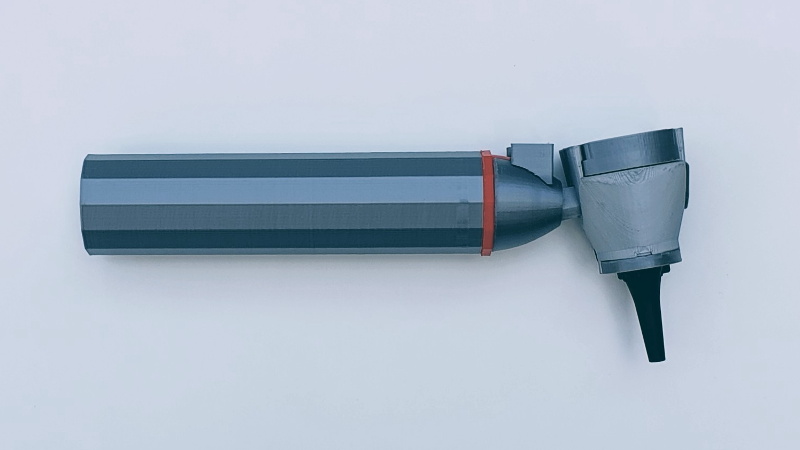
 Glia member [Tarek Loubani] has recently written a blog post discussing the team’s latest release: an otoscope that can be built for as little as $5. Even if you don’t recognize the name, you’ve almost certainly seen one of them in use. The otoscope is used to look inside the ear and can be invaluable in diagnosing illnesses, especially in children. Unfortunately, while this iconic piece of equipment is quite simple on a technical level, professional-quality versions can cost hundreds of dollars.
Glia member [Tarek Loubani] has recently written a blog post discussing the team’s latest release: an otoscope that can be built for as little as $5. Even if you don’t recognize the name, you’ve almost certainly seen one of them in use. The otoscope is used to look inside the ear and can be invaluable in diagnosing illnesses, especially in children. Unfortunately, while this iconic piece of equipment is quite simple on a technical level, professional-quality versions can cost hundreds of dollars.
Now to be fair, you’ll need quite a bit more than just the 3D printed parts to assemble the device. The final product requires some electrical components such as a battery holder, rocker switch, and LED. It also requires a custom lens, though the Glia team has thought ahead here and provided the files for printable jigs that will allow you to cut a larger lens down to the size required by their otoscope. In a situation where you might have to improvise with what you have, that’s a very clever design element.
So far the team is very happy with how the otoscope performs, but they’ve run into a bit of a logistical snag. It turns out that early work on the project was done in the web-based TinkerCAD, which isn’t quite in line with the team’s goals of keeping everything free and open. They’d like some assistance in recreating the STLs in FreeCAD or OpenSCAD so they’re easier to modify down the road. So if you’re a FOSS CAD master and want to earn some positive karma, head over to the GitHub page for the project and put those skills to use.
We’ve previously covered Glia’s work with 3D printed tourniquets to treat gunshot wounds, a project that led to [Tarek] himself being shot by a sniper while attempting to field test the design in Gaza. If that’s not commitment to the principles of open-source hardware, we don’t know what is.













This is great. Medical stuff is insanely overpriced, even when the regulatory requirements are not so onerous as to remotely justify it. For my third year in medical school I got a cheap LED penlight, but an attending said it was “too blue,” which to be fair was true, it had horrible color rendering index. So I got a halogen one from Welch-Alyn, one of the big names in medical devices. It worked fine, battery life notwithstanding, until one day I dropped it and the bulb burnt out. When I went to get a replacement, they wanted over thirty dollars! They had designed it so that the bulb was integrated with a machined and anodized metal part, such that there was no easy way to just replace the bulb itself. Outrageous. I ended up getting a high-CRI LED light from a non-medical supplier, it’s been great so no regrets other than wasting my money on the Welch-Alyn one.
That’s an outrageous story, [Bryce]. With the base we’re building for this Otoscope, we should be able to parlay it into other simple devices like a pen light. The advantage would be that Glia can put it through the regulatory process and get it certified as a Class I medical device (Health Canada right now, but we’re working on CE and eventually FDA).
While you and I both know that doesn’t usually matter, it is the difference between being allowed to use it on patients in a clinical setting and not.
If you send the exact Welch Allyn penlight you used, we could put it in our back pocket for when we have a bit more time to work on this.
tarek : )
Ah, nothing like a perfect place to raise bacteria. I wanted to 3D print a toilet seat but as it turned out pieces of fecal matter would be stuck between print layers. This device, while innovative is just like my toilet seat – you can’t just clean it, the plastic itself is stained by now. You’d have to replace an entire seat.
It seems to be using an off-the-shelf disposable plastic speculum for the patient-contacting part. If you’re worried about the handle, try not to think about the doctor’s white coat. Seriously though, this is definitely an issue with 3D printed stuff, but it’s not intractable. You could sand or vapor polish it to improve the surface finish, for example.
Or you could coat it with paint etc.
plastidip the handle maybe?
polyurethane is probably not the best idea… you want something hard, that’s difficult to imbed things into – paint and a hard clearcoat. Needs a lot of prep though.
Why worry about the coat – it is white so it is easier to bleach. (Of course lots of idiots wear scrubs out where they shouldn’t, so hard to tell if they are contaminated or not – either taking pathogens out of where they should stay, or in to where they shouldn’t be.)
Thing to really worry about is their cell phones (or other com devices). NIH found they had to take cell phones away from care-givers in wards where dealing with nasty bugs, you can’t get people to stop touching their phones, and they don’t get cleaned near enough.
When somebody comes into your hospital room and washes their hands – thank them for that, but if they then touch their phone – ask them if they cleaned the phone since the last patient (or ask them to wash their hands again).
(The control for the TV/etc. Same thing.)
Hospital-provided scrubs that you can’t take home with you are probably the best thing for this. As to just bleaching the coat… I don’t know what country you are in, but at least in the USA doctors are way too busy to be doing laundry every night, so it would have to be through the hospital laundry service. I mean, that’s the way I’d do it if I were running a hospital, but not every hospital does this. In a lot of them, doctors are responsible for buying and maintaining their white coats and hospital-provided scrubs are only available to proceduralists. NHS in the UK has even gotten rid of white coats, or so I hear, because of their potential to transmit infection.
Good point about cellphones (and other devices) – I often see people gown and glove when going into rooms with infection controls in place, but then touch penlights, phones, pens, notepads, etc. The hospital provides some kind of disinfectant wipes for that stuff, but sometimes people forget to use it… also it doesn’t really work on paper for obvious reasons.
Thanks for giving us the chance to discuss this myth. As [Bryce] mentions in this thread, we use disposable specula to contact the patient. The handles.. well.. Like [Bryce] said, try not to think too much about that. I can’t remember the last time I saw a doctor wipe hers / his down with anything.
However, there’s been a significant amount of work done on the issue of sterilizable 3d printed parts. The canonical whitepaper may be biased (it’s by Stratsys), but it is thorough and generally cited: https://www.meddeviceonline.com/doc/sterilization-of-d-printed-medical-devices-0001 . You need a free signup to see the whole paper.
To summarize, there are broadly 4 commonly used techniques for sterilization of medical equipment: autoclave, ethylene oxide, hydrogen peroxide, and gamma radiation.
For simplicity, let’s dismiss autoclave (high heat) since it warps samples. Printed samples sterilized with all three of the other techniques showed essentially no growth in a broth after 14 daus (1 out of 180 of the remaining samples showed growth).
The closest thing used in clinical practice to any of those techniques is probably accelerated hydrogen peroxide wipes, which is probably good enough to deal with the problem. Of course the goal is not sterility with a non-sterile device like an otoscope, but just keeping it generally clean.
I hope that clarifies things. Thanks for raising the issue!
tarek : )
Try reading, or even just looking at the pictures. It uses the same disposal tips as the commercial ones.
Well since they’re building these for the third world why not go for something more primitive, like Brunton’s auriscope, it could be as easily printed and can work with an ordinary flashlight, lamp or candle. Here is a picture of the original one.
http://otoscopy.hawkelibrary.com/album09/GS_10
Thank you for your suggestion, [Hirudinea]. I’m one of the people involved with the otoscope design, and we took a hard look at other designs as well previously. One of the decisions we made was to try to create FLOSS drop-in replacements. The auriscope you describe is not used by modern practitioners for several reasons:
1. It doesn’t allow for disposable ocular specula – the cone thing that touches the ear. Most modern infection control departments would simply not allow a device with a reusable speculum in at this time, rightly or wrongly. I agree that the net harm of disposable specula is greater than the benefits in terms of environmental / societal vs. individual impact, but this is not in my wheelhouse.
2. It would require a modification to insert the 3x magnification currently used by practitioners. Unmagnified tympanic membranes can mean that we miss subtle tears or air bubbles (an indication there’s fluid in the middle ear).
3. Most doctors no longer carry pen lights or flashlights with them, and these would have to be controlled for intensity and spectrum delivery as noted in a comment above so as to give reliable and valid results. In fact, part of the redesign in version 3 was the recognition that most doctors use otoscopes *instead* of pen lights, so a modification was made to allow more clarity when examining throats too.
4. Pneumatic otoscopy is difficult or nearly impossible with these. While not that many of us use pneumatic otoscopy any more, it’s usually a purchasing criteria for the rare case where we have to see what the tympanic membrane is doing. This is where air is blown into the outer ear to see how much the tympanic membrane moves.
All of these problems can be remedied if you modify Brunton’s Auriscope. But then you end up with the modern design. Also, it’s hard enough getting people to take this kind of work seriously. It’s one reason we try to stick to the things people know, especially in a conservative sport such as medicine.
tarek : )
I paid 99 cents (shipping included) for an ear cleaning device that is even simpler.
It has an LED, a watch battery, and a transparent plastic cleaning pick. The LED shines into the base of the plastic pick.
No special mirror needed.
Just glue the pick to the inside of the plastic speculum and you’re done! If you need magnification: reading glasses.
I think that 3x magnification won’t always be necessary, I’m not a doctor but I expect slightly higher or lower magnifications could be used, although focal length will probably be important. To that end, I think designing multiple styles of lense holders to accept several styles of eyeglasses lense would make the otoscope easier to make in the field. it might even be possible to make a “universal” lense holder that holds most rectangle style lenses, in terms of function I don’t think it really matters if a bit of the lense overhangs the body of the device as long as there aren’t any sharp edges.
I don’t work with 3D printers but I expect some filaments have some spring to them which when combined with a metal pad should make the battery holder mostly 3D printable as well.
with a bit of 10 gauge or thicker wire I could see mushrooming an end on a small section of it, passing it through a hole on the springy bit of the battery holder then soldering a wire to the non mushroomed end, the mushrooming would prevent the contact from slipping through the hole, and the springy bit of the holder would push keep the mushroom in contact with the battery.
I wonder how well PET would work for the print, because using a plastic beverage container to make the device would be an great ability to allow for production just about anywhere, especially where there is an ocean beach.
Those are just my thoughts on posabilities, feel free to shoot them down if I’m completely off base as I wouldn’t like someone to take my opinions as fact and do something dangerous/stupid/wrong. :P
Hi [dscrive],
Thank you so much for your comments! I’ll tackle them one by one.
– 3x magnification: We really just matched the modern otoscope as much as possible so people could use these otoscopes in mixed environments and not need any retraining. I suspect you’re right that 2.5 – 3.5x would be fine, but I would defer to the audiologists on this one. 3x is plenty easy to find, though, so not a huge deal to stick to spec, especially because we want to help people gain regulatory certification and we can’t guarantee the other variants will work as well as the ones we release.
It’s annoying to cut down the lenses for sure. However, most places probably only need about 1 otoscope for 10,000 people in the catchment area, so we’re talking about 200 otoscopes for a place with 2 million people. Generally those kinds of numbers will need standardization for a number of reasons, and the situation in – while dire in some places – permits for 200 of a particular lens. Our lens is recruited from a commonly available magnifier thing that is easy to move around and doesn’t trip import/export red flags, so it’s not a huge deal. We’re experimenting with cheaper 3x lenses purchased from aliexpress / amazon / ebay / etc.
Our target demographic isn’t committed hobbyists making one-offs, but ministries of health and national governments. Hobbyists, engineers and clinicians serve critical roles in development, testing, refinement, etc. At the end of the day, though, a health system has to buy in through their ministries, health units and hospitals or it won’t work.
– battery holder: Great idea. This is outside Frankie’s scope (the original designer), but we hope that once we get this working, we can do some effective engineering to reduce the complexity of the devices and the external dependencies. Your ideas are worth exploring and I’ll pass them along. Thank you.
– PET: There are lots of kinds of PET. We use ABS in most low-income places we operate and PETG in rich countries where it’s available. In one of Glia’s major low-income hubs (Gaza), ABS is captured and recycled from the waste stream. They have an almost 100% recycle rate on all plastics there, which is by necessity since virgin plastic is banned from entry except as packaging. We guard our virgin pellets that occasionally enter and use as little as possible while pulling filament.
Printing PETE (the bottles you’re thinking of) is reaaaaallly hard. I think T-Glase by Taulman 3D is really the only one I can think of that has succeeded with this. I don’t see any great reason to go for PETE when they recycle it to other purposes and we have ABS there.
Thank you for your comments and feedback. It’s really valuable to hear your thoughts on how we can improve and to channel those suggestions to the team!
tarek : )
I like your idea about using lenses from reading glasses!
Speculum, Reflex Hammer, Woods Lamp and a Micro/Endo/Colposcope come to mind as easy devices to build and I didn’t notice on the git. Dilators, Retractors and Stereotactic tools wouldn’t be too complicated. A trocar would be interesting and more complex.
Wondering what is most needed in the field and would be best to prioritize?
Hi! These are all really fantastic ideas. Other groups have made gynecological specula (See GynePunk). The other devices are indeed simple and on our list. Surgical retractors have been made by others and tested as well, and we tried to reach out to the author. For now, we’re focusing on devices others haven’t made, and then hopefully going to bring their devices in and ensure they’re part of a FLOSS repository of devices that institutions can use and that we can curate as clinical- and liability-grade.
I think probably surgical tools like retractors, scalpel blade holders, clamps would be a great next project that we’ve started and stopped several times and don’t have a good clinical and engineering lead for: https://github.com/GliaX/SurgicalTools/
If this is something you’re really interested in, send an email along to discuss more at info@glia.org
tarek : )
“Wondering what is most needed in the field[…]”
Bone splints/casts? (adjustable, of course) IMHO
Traction devices to field improvise easier somehow?
Very well timed article!
I am in the process of being booked to take my 3D printers to the local hospital to demonstrate their operation.
This will be a great addition to the stethoscope I’ve printed already.
It would be great to hear more about your work with the hospital!
tarek : )
You should poke https://www.facebook.com/drsusanjewellMD for more designs.
Is it better than the 3$ Otoscopes you can buy shipped from china?
Yes. These are more or less equivalent to the $400 models. If we can make the focus adjustable (a stretch goal that I don’t think we need to aim for), they will become equivalent to the $1000 models.
The key characteristics are: optics (how well you can see things) and light clarity (how well the light shines). The last one being the ability to take on different disposable specula. Our current model takes Welch Allyn, but it would be trivial to change it as needed to the different manufacturers, functionally commodifying the specula and killing vendor lock-in.
tarek : )
@Tarek Thanks a lot for all your answers in this thread. You gave a lot of interesting insight into this topic that I missed from the original article. Thank you for being dedicated to this good cause. I wish you all the best.
Wow, please don’t! An otoscope needs to be cleaned every once in a while and a certain robustness. This is clearly a project mostly driven by a solution looking for a problem. Otoscopes are already dirt cheap, around 7 to 20 bucks depending on style and durability, and last forever.
For all those times when you have a 3d printer and all the feedstock and spares to operate it, but no basic tools. Right.
I must be missing the point or something. For the price of a reliable 3d printer, I can buy bushels and bushels of cheap Chinese medical equipment that’s arguably better, at least the surfaces are smooth and cleanable.
Yes, you are. Had you bothered to read the posts from Tarek (the guy actually in the field developing this stuff), you’d know the answer.
I’ll give you a hint. Amazon Prime isn’t delivering to a warzone, and by the time the slow boat from China gets there with your gear, the patients are dead already.
And 3d printers are so wonderfully robust and sturdy that they are easy to come by and operate in a war zone?
Our practical experience in Gaza says yes. We have about 20 printers in our office there that are run with solar power (power is as low as 4h/day and Israel just halved the power plant’s diesel it allows in yesterday). Our filament is produced from recycled ABS put through a filament extruder we made locally when we retired our hardworking filastruder.
There are some sister projects coming up in other countries with different problems, so within about 10 years we can answer this question definitively. For the time being, though, the project has created lots of direct and indirect benefits to my patients in Gaza and Canada and seems worth continuing.
tarek : )
1. How many third world countries have greater access to 3D printers than to basic medical tools?
2. Why would anyone invest in the 3D printer in third world country, when for example cheapest otoscopes sell for less than 2USD with free shipping, and stethoscopes sell for less than a buck?
3. Long time ago people made medical instruments from wood, steel, glass and rubber, sometimes in their kitchens. First artificial kidney that actually worked used cellophane sausage skins and hydraulic fluid bearings from fighter planes.
Just because everyone in the west has 3D printer doesn’t mean that they can be found in every poor country in the world. Some countries struggle to get good supply of drinkable water, I don’t think 3D printers will be high on their priority list…
Yea I’m not buying this either. I could see the utility in ‘here are a bunch of completely printable medical things’ for situations where you happen to have a 3d printer and someone starts blowing up your country. But at the point where you’ve had the foresight to buy all the *other* parts needed, you might as well have bought the gear itself. Considering the guy decided to go into an existing war zone and try to test stuff, this smells like a solution in search of a problem. Maybe it should be solved with blockchain!
I see the point that people are making about not having 3D printers where you need them for this. It might be a fairly narrow range of places where this is applicable… places that are technologically sophisticated but under blockade for example. It might also make the most sense to target things that can benefit from customization to the patient, for example orthotics as mentioned above.
The particular case here is in Gaza, where Israel forbids the import of certain medical devices but 3d printers are available. Also while it is quite possible to make say an otoscope from plumbing pieces or to whittle a stethoscope head both of these require a certain amount of technical skill in handling the materials/parts and an ability to adapt pieces to allow nonstandard uses. The use of a 3d printer minimizes the need for the manufacturer to be able to shape or modify parts, it’s all press fit and glue. even the soldering of wires could probably be avoided. I think this is a great project and have contributed to the work on the tourniquet as well.
Thank you for this! It’s a great point that medical devices need consistency and shouldn’t need artisans to make them. I agree with you that the otoscope can be simplified, and this is a goal of ours as the project progresses. Frankie, the original designer, did a great job, but he’s an audiologist, not a manufacturing engineer. No doubt we can reduce the cost and labour required with a bit of effort.
tarek : )
Thanks for raising this important concern, [Myorc]. We should always be careful to start from the ground and work our way up. I am a clinical emergency physician who works on the frontlines. I work in the Gaza Strip currently (since 2011), but I delivered care during a massacre in Egypt, during incursions in the West Bank, during the war in Iraq (Fallujah and Baghdad), in the post war period in South Lebanon, in rural Colombia and in the capital of Venezuela. I’ve also attended as a medic in numerous street protests in Canada. I’ve participated in wide infrastructure projects (e.g., solar power on hospitals) as well as physician and nurse training in the places above. In Canada, as well as a clinical role treating patients in the emergency department, I have an academic role in teaching medical students and residents and also as the medical director of our region’s advanced cardiac life support program that teaches doctors how to respond when patients’ hearts stop or almost stop.
Glia’s medical director is Gaza’s first locally board-certified emergency doctor, and treated thousands of patients in three massive wars and countless “mini wars”, as well as being one of the key pre-hospital and disaster medicine organizers in Gaza.
In short, we’re not doing this project to fuck around. We’re doing it to save our patients’ lives and deal with real issues.
I’d like to tackle your comments one by one.
1. All of them. In Gaza, we use clones of Prusa’s i3 MK2/3. We started with i3’s in 2015. Gaza is hermetically sealed by an intense military / economic blockade, but we were still able to get a printer in and then use it to print others. At this point, there are at least 50 printers I’m aware of, all of them locally made. The RAMPS and hotends are the hardest parts to source, but some (not so good) hotends are even being produced locally. I assume you have very little experience with 3D printers such as the Reprap’s descendants of which Prusa is one. They are very easy to source parts for and to make from scratch. Many parts for modern printers can be printed, and the designs are resilient to scarcity of almost any part.
The flip side of your question is about medical tools and their availability. Glia’s motto – “equal care” – says it all. If you assume – as we do – that third world patients deserve the same medical devices and tools that people in rich countries deserve, then it’s easy to recognize the massive shortages of devices and tools. In Gaza, currently 40% of essential medications are absent. Devices are so pervasively short that the only supplies that are even counted are gauze and sutures. The rest are assumed to be stocked out and in constant need of purchase as available.
2. I’m curious how much you think a 3D printer costs. In Canada where we buy Prusa kits, the cost is CAD$1000 (let’s call it USD$750) shipped and through customs. We just took our lab to 10 printers recently, so this figure is within the last few months. In Gaza, where we source everything locally ourselves, they cost about USD$200 since most stepper motors are salvaged from other parts. There are many good reasons, but let me expand on two:
a. Creating a domestic medical device industry is A Good Thing. By reconfiguring the relationship from consumer-user to creator-user, we encourage innovation in the devices. Customizability to fit for purpose is one aspect – the needs of Gaza are different than Toronto. But also creating these devices in the open and manufacturing them locally allows for overall downward pressure on the costs of premium medical devices. Most of the cost of medical devices is profit and marketing even after accounting for R&D costs. Similarly, creating that set of local experience (CAD, manufacturing, etc.) will have lateral effects as student volunteers, trainees and employees leave local medical device production and go into other industries. It’s not just medical devices that are short in Gaza and other poor countries. It’s everything.
b. Why don’t I or my colleagues in Canada use these $2 otoscopes shipped for free? I’m not paying for any of these devices, so I don’t care if they cost $2 or $1000 (the cost of the units I use in practice). Administrators who buy in bulk and care only about dollars are making purchasing decisions. So why don’t they go for the cheap units?
Because they SUCK.
If I can’t do my job and miss problems in patients, the cost to the system goes way up. Similarly, if half of the units are broken, then the inventory / stocking / repair budget will increase such that the total cost of the unit goes way up (a concept called Total Cost of Ownership). We’re not trying to make low quality versions of devices that desperate people are forced to use. We’re trying to make high quality versions of devices that are low cost and people *want* to use.
Generic hardware manufacturers are trying. But they don’t have plans for high quality devices that are validated and approved by health bodies, which is why most of those devices are very poor quality. By releasing our devices as open source, we invite these generic manufacturers to use them instead of developing devices in-house. We clinically validate all our devices and have literally published a paper in a peer-reviewed journal showing the quality of one of our devices is equivalent to the most expensive premium brands. That work cost tens of thousands of dollars and I’m not surprised generics manufacturers aren’t doing it.
We’re working on validating a pulse oximeter right now and the total cost of that project is upwards of $200K, a significant amount of which I contributed personally. These are hard problems.
3. I’ll assume that you’re making this comment in earnest, though the tone intimates otherwise. We have lost some things to modernity, but there’s no disputing that health outcomes today are much better than ever before. During the imaginary golden age of medicine you hearken back to, doctors also did rectal examinations without gloves. As the doctor in that scenario 99.99% of the time: No thanks, I’ll take the gloves. The real trick is to try to reduce medical tools to their essential parts and figure out what is needed and what is extraneous. That’s at the heart of this project. For now, though, until much more research is done on sterile manufacturing (we have animal studies planned to test some of these concepts since sterile manufacturing is not possible in most of these places), my professional suggestion to you as a doctor is that you shouldn’t accept kitchen medicine for yourself. And if it’s not good enough for you, it’s not good enough for poor people either. But don’t worry, I’ll get off your lawn soon.
4. According to the Palestinian Central Bureau of Statistics in a 2018 report, about 89 per cent of the population of Gaza does not have access to safe drinking water. Tania McBride, the chief of UNICEF’s Gaza Field Office, was reported as saying less than 4 per cent of Gaza’s ground water is usable. Kids are getting sick and dying every day from bad water. Like many in Gaza, I get rashes from the water when I shower and get a bit nauseous when raw sewage is being dumped in the sea in the mornings close to where I’m staying. What does this straw man argument have to do with medical devices? I have dirty water so I should just give up? Don’t try to solve any problems until the water problem is solved? I’m not following.
tarek : )
“The idea of cheap interchangeable devices for the 3rd world countries suffering from war is just fine.
We are not talking about the highest grade equipment. We are talking about necessary equipment. Equipment that will save lives right then and there.
Lately there has been a big move toward smaller hospitals in America buying used equipment. Instead of the newest best stuff out there.
And even that move has saved the lives of countless millions in the last 8 years since the small hospitals have always had a problem obtaining the equipment they needed.
I remember the last group of used medical equipment our small hospital in Idaho got in came from the Mazree.com auctions. And some came from eBay. You should have seen the movers bring the C Arm machine in. And we were grateful to have it.”
I’m curious who this quotation is from. In the countries I have worked in, the “anything is better than nothing” mentality is not the one I find. While I can see why people might think so, it diminishes the people who are involved reinforces donors thinking that those who receive donations are second-class citizens. Never mind the huge practical problems that are almost always associated with this mentality.
Yes, we could have gone begging and picked up the scraps of the first world. Instead, we spent the money creating our own alternatives. We’re better for it in Canada, Gaza, and everywhere else.
Everybody deserves equal care.
tarek : )