It’s rarely a wise idea to put a plastic bag over one’s head, but when the choice is between that and possibly being exposed to a dangerous virus, you do what you have to. So you might as well do it right and build a field-expedient positive pressure hood.
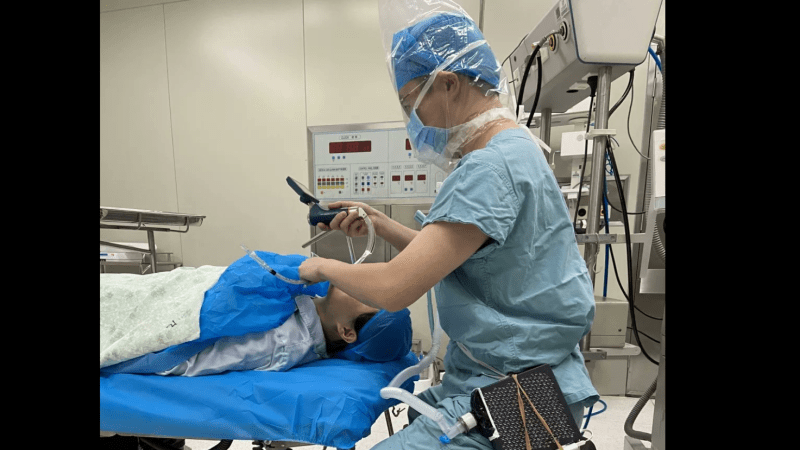
We’ve all been keeping tabs on the continuing coronavirus outbreak in China, but nobody is following as closely as our many friends in China. Hackaday contributor [Naomi Wu] is in from Shenzhen, posting regularly from the quarantined zone, and she found this little gem of ingenuity from a [Doctor Cui] in one of the hospitals in Wuhan. Quarantines and travel restrictions have put personal protective equipment like masks and gowns in limited supply, with the more advanced gear needed by those deal most closely with coronavirus patients difficult to come by.
There’s no build information, but from the pictures we can guess at what [Dr. Cui] came up with. The boxy bit is an AirPro Car, a HEPA filter meant to clean the cabin air in a motor vehicle. He glued on a USB battery pack to power it, used a scrap of plastic and some silicone adhesive to adapt a heat-moisture exchange filter from a mechanical ventilator to the AirPro’s outlet, and stuck the tube into a plastic bag sealed around his neck. The filter provides dry, positive pressure air to keep the bag from fogging up, and to keep [Dr. Cui] from asphyxiating. Plus he’s protected from droplet contact, which is a big plus over simple paper masks.
With the news always so dark, it’s heartening to see stories of ingenuity like this. We wish [Dr. Cui] and all our friends in China the best during this outbreak.













That’s a cool hack. But, how come he’s not wearing gloves?
as long as he has no cuts on them and he washes them before touching anything else, he doesn’t really need them…
I understand that, but that seems like an easily mitigated unnecessary risk to take when dealing with infectious diseases.
It’s possible that coronaviruses can’t survive, much less replicate, in a cut or other wound-type entry. They express proteins that bond to specific cell surface receptors, and probably don’t handle epithelial tissues covered in t-cells very well. What they want is water-moist mucous membranes.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3397359/ has more details.
I’m not saying gloves are a bad idea, but if he’s convince they’re not useful for his care and they’re in short supply, he may be leaving them for other health care people whose exposure pattern is more infectious.
Great he wont have coronavirus. Just the HIV and Hep C….
This seems to be moulage not a live case.
They probably ran out of gloves *very* quickly since many Chinese hospitals were inundated with patients.
“Quarantines and travel restrictions have put personal protective equipment like masks and gowns in limited supply,”
I would assume that includes gloves as well.
Bingo
Gloves in a can™.
I think that is a dummy (even it’s not moulage I’m sure it’s not really someone he intends to tube) and not a live person. He is probably practicing procedures wearing this device to make sure it doesn’t interfer with his work too much.
I am sure he will be wearing gloves in a live scenario and this is staged for the photo.
Gloves can be counter productive in situations like this. The best protection against corona viruses is good hand hygiene. When humans wear glove they are less likely to wash their hands as thoroughly.
Finally someone with some sense. I know of well regarded labs where gloves are banned for the very reason you mention. It’s about achieving the goal effectively and that’s not always as straightforward as people’d think.
Now that is some clever use of materials on hand! Kudos to Dr. Cui!
I hope that he and all of the others affected by this outbreak will be able to either avoid getting sick or return to health quickly.
As I recall, the same setup was used onboard Apollo 13.
https://youtu.be/ry55–J4_VQ
Naomi Wu is not in China and hasn’t been for a while, she made a video about this very thing to let people know she’s safely away. She got the pictures from an article, there’s a post from her lower down with the link: https://t.co/BBo7Wt1Pvx
My mistake, I missed her post saying she’s in Thailand. The article has been corrected.
It is likely they are out of gloves. Supplies are a bit strained due to the overwhelming volume of need. Often these folks are doing the best they can with what they have.
For a ,producer to the world, country that’s saying a lot.
Taking out shabby dusty insulation and putting in new on a friends garage, I thought of this. Hosing in fresh air into a hood or helmet instead of hoping a mask works with it’s discomforts that send fingers after itches.
Yup. I was reading somewhere they were retooling other industries to produce masks and such. I’m definitely rooting for em to overcome.
The AirPro is a PM2.5 filter.
Unfortunately, the Coronavirus is substantially smaller than a PM2.5 particle, so this filter probably does nothing.
Bu this would be great for keeping your lungs clean when sanding.
the article here says “HEPA filter”, which contradicts the linked airpro model. *shrug*
We have the “Hepa” and The “Hepa Absolute”.
Choose wisely..
Like any advertisement, they probably play loose and fast with the facts. But it says HEPA, so I said HEPA. Maybe it’s not up to ASME standards, but it’s a whole heck of a lot better than his alternative, which is nothing at all.
Most people are using a simple surgical mask or an ill-fitting N95 mask at best to protect themselves from coronavirus. I think PM2.5 is a huge step up over that, and way better than going in with nothing.
I couldn’t find easy data on this, but this site (selling their own filters) claims pita and PM2.5 masks are useless: https://smartairfilters.com/en/blog/pitta-masks-protect-capture-coronavirus-virus/
However, as a friend who works in virology pointed out, any mask is useless if it doesn’t fit and doesn’t cover your eyes, which this at least does.
Another advantage is that the input air is coming from a long way from the patient’s sneezy mouth, so there will be less contamination to start with. Also the viruses themselves may be << PM2.5, but what about the droplets they are in? If you can eliminate a good proportion of the droplets you're winning. This article https://www.ncbi.nlm.nih.gov/books/NBK143281/ suggests that he'll catch most of them.
Wow, that article is a lot more encouraging on the effectiveness of masks.
Good point also about the source of the air being further from patients, though that will be dependant on there not being too many patients around – so maybe not a benefit on the subway for example.
“Coronaviruses are mainly transmitted by large respiratory droplets and direct or indirect contact with infected secretions. They have also been detected in blood, faeces and urine and, under certain circumstances, airborne transmission is thought to have occurred from aerosolised respiratory secretions and faecal material.” – UK official guide
“Published data have suggested that sneezing may produce as many as 40 000 droplets between 0.5–12 μm in diameter […] whereas coughing may produce up to 3000 droplet nuclei, about the same number as talking for five minutes.
“[…] found that, under normal air conditions, droplets smaller than 100 μm in diameter would completely dry out before falling approximately 2 m to the ground” – https://www.ncbi.nlm.nih.gov/books/NBK143281/
I recommend to take a look at the falling curve in the article above… it shows, droplets in room temp smaller than 100μm dry out pretty fast, so smaller thatn 2,5 dry out very fast.
Question remain: how long the dried out small particulate circulate, how long are the viruses yet virulent when dried out, but a PM2,5 Filter + physical barrier to face seems for me to do the trick very well.
the heat moisture exchange filter is actually to humidify the air
Maybe Chinese people should stop eating bats, rats, anteaters, dogs, etc.
They think it’s pangolins this time, which are already illegal in China.
Is there any Biochemical labs in Wuhan ??