Throughout history, the human body has been the subject of endless scrutiny and wonder. Many puzzled over the function of all these organs and fluids found inside. This included the purpose of blood, which saw itself alternately disregarded as being merely for ‘cooling the body’, to being responsible for regulating the body’s humors, leading to the practice of bloodletting and other questionable remedies. As medical science progressed, however, we came to quite a different perspective.
Simply put, our circulatory system and the blood inside it, is what allows us large, multi-celled organisms to exist. It carries oxygen and nutrients to cells, while enabling the removal of waste products as well as an easy path for the cells that make up our immune system. Our blood and the tissues involved with it are crucial to a healthy existence. This is something which becomes painfully clear when we talk about injuries and surgeries that involve severe blood loss.
While the practice of blood transfusions from donated blood has made a tremendous difference here, it’s not always easy to keep every single type of blood stocked, especially not in remote hospitals, in an ambulance, or in the midst of a war zone. Here the use of artificial blood — free from complicated storage requirements and the need to balance blood types — could be revolutionary and save countless lives, including those whose religion forbids the transfusion of human blood.
Although a lot of progress has been made in this field, with a limited number of practical products, it’s nevertheless proving to be a challenge to hit upon a replacement that ticks all of the boxes needed to make it generic and safe.
Not Just Any Fluid

Although there are reports of the Incas practicing blood transfusions between humans as far back as the 16th century, it wasn’t until William Harvey (1578 – 1657) described the human circulatory system and the properties of the blood in 17th century that the modern views of this aspect of human physiology began to take shape. This came alongside blood transfusion experiments primarily between animals.
In 1665, physician Richard Lower performed a crude blood transfusion between two dogs, with apparently no ill effect on either animal after said procedure. Around this time blood transfusions from an animal into a human (xenotransfusion) was also attempted, with many of the human subjects not surviving the procedure, presumably due to the body’s rejection of this foreign blood.
Similar issues as with xenotransfusion cropped up with blood transfusions between humans: while sometimes this would work, other times the receiving subject would suffer ill effects and some would die as a result. This led to blood transfusions having a poor reputation in the 19th century. It wasn’t until 1901 when Karl Landsteiner discovered the three human blood groups (A, B, O) that an explanation for these results became clear.
When incompatible blood types are mixed together, one could observe clearly how the red blood cells would clump together. It was at that point easy to imagine what would happen inside the human body if such a response were to occur during a blood transfusion. This insight led to the first of many revolutions that would make blood transfusions as safe and commonplace as they are today.
Copying from a Master
The obvious complication with trying to replicate the functionality of human blood is that we’re trying to recreate something that has evolved over millions of years, inside a larger system (the body) which relies on its many aspects to function just right. Even if it is not intended to be in the body for longer than needed until natural blood levels have recovered, it cannot be allowed to cause more harm than it prevents.
In humans, blood accounts for ~7% of total body weight. Its density is around 1060 kg/m3, which is very close to the 1000 kg/m3 of water. An adult human has on average about 4.5 L of blood, which consists of ~45% out of red blood cells, ~54.3% plasma, and roughly 0.7% of white blood cells. Generally speaking, each of these form the three main function groups of blood.
Red blood cells contain hemoglobin, which bind oxygen, white blood cells (along with antibodies) form a major part of the immune system, and plasma contains the nutrients, electrolytes and blood-clotting factors that sustain cells and allow for the repair of injuries through coagulation. From this we can deduce what is required in a blood substitute: crucially the functionality of red blood cells, along with a carrier fluid akin to plasma (which is ~95% water).
While the latter is relatively straightforward in the form of crystalloid solutions (e.g. saline solution), the complexity comes with substituting the functionality of the red blood cells. Here two approaches have seen major research and (limited) use: perfluorocarbon- and hemoglobin-based oxygen carriers (PFBOC and HBOC, respectively).
Binding Oxygen, Loosely
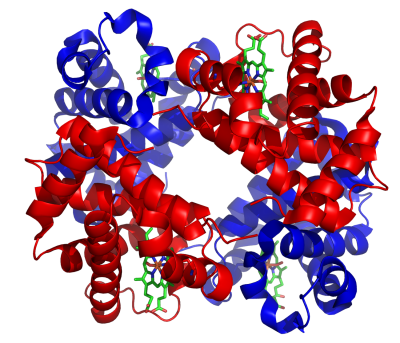
Where an oxygen carrier with the characteristics of red blood cells become complicated is that these molecules should not just bind to the oxygen, but they should also easily make it available to the body’s tissues. An obvious thought here would be to synthesize hemoglobin and use that directly. The snag is that hemoglobin by itself has a very high oxygen affinity, has a short half-life in the blood, and can damage the kidneys. In a red blood cell (RBC), hemoglobin makes up only 33% of the cell’s mass, with the remaining mass acting to stabilize the hemoglobin.
For this reason an HBOC using plain hemoglobin would be useless, as it would not provide enough oxygen to the tissues. To resolve this, the hemoglobin has to be stabilized in a way that still allows for the binding to oxygen, while not inhibiting the distribution to tissues. A number of companies have undertaken efforts to bring such HBOCs onto the market, with HemAssist (by Baxter Healthcare), Hemolink (Hemosol, Inc.) and Hemopure (Biopure Corp) and others either failing during trials, or shortly after entering commercial sales.
Common issues observed include vasoconstriction, presumably due to the hemoglobin binding to nitric oxide. Most of these HBOCs were targeting use in non-human animals, where increased mortality led to these products not passing medical trials, or being pulled off the market within a few years.
In contrast, there is one FDA-approved PFBOC: Fluosol-DA, with e.g. Sutherland et al. (1984), reporting on its effectiveness with cats, and Ohyanagi et al. (1984) on the effectiveness of Fluosol-DA 20% infusion with Jehovah’s Witness patients. As in the latter group’s religion leads them to refuse blood transfusions and similar, this can be problematic with medical care.
Even so, the complexity of Fluosol — patients must breathe a pure oxygen atmosphere to ‘load’ the PFBOC molecules with enough oxygen — and its complicated storage (freezing) and handling requirements led to production ceasing in 1994.
Not Bled Out Yet
Despite the many setbacks over the years in getting a solid blood substitute onto the market, the need for such a solution is too immense for research to cease. This leads us to current developments, with the US military being one of the interested buyers for these blood substitutes. Not just for oxygen carriers, but also for synthetic platelets (for coagulation) and dried plasma.
The main selling points here are an increased shelf-life, the removal of complicated matching of blood types, reducing the possibility of allergic reactions, and so on. Although we have come a long way from the early days of blood transfusions, we still rely on blood donations, and the system that processes this blood. While it’s a system that saves countless lives each year, it comes with the disadvantages of complex logistics, short shelf-life, and the possibility of contaminated blood.
Synthetic blood has the advantage here that it can be produced in any desired quantity and under strictly controlled conditions. An added advantage of e.g. PFBOCs is that they feature much smaller molecules than RBCs, which allows them to bypass even blockages and constrictions in arteries. This would allow for oxygenation of tissues that’d otherwise end up being oxygen deprived and die, which can prevent necrosis, amputation, and other complications of traumatic injury.
Sci-Fi Until It’s Reality
Although the optimism of the late 20th century about blood substitutes seems to have quieted down after so many setbacks the past decades, there are a lot of things which we have learned about not only what doesn’t work, but also what does. We also gained a lot of important information on aspects of human physiology, which serve to increase our understanding of the cardiovascular system.
A few hundred years ago, people thought that sheep’s blood or even wine or urine would make good substitutes for human blood. Today we understand many of the complexities of blood type determination, can process donated blood to use only the RBCs, plasma or platelets, to treat a number of medical conditions, and so on. With blood substitutes having been reduced to mostly a medical engineering question, chances are that we may see progress here before long.















And feeding vampires, don’t forget to build in vampire nutrition. Think of all the countless virgin lives that could be saved by a good artificial vampire smoothie!
There ain’t no vampires anymore.
We ran out of virgins during the Hippy Free Love movement in the 1960s>
You can thank my generation later… :)
Thanks boomer.
One of the things about free love is that you make plenty of virgins.
TRUE!!! Nothing else tastes quite right…. we need a viable alternative so i can spend less time hunting for dinner and more time hunting for a Ber Rune…
If we implement LastDay, then when people go to Carousel they can suck out their blood first. Though since longevity is brought by blood transfusions in part, you need less spare blood if people are terminated at 30
Ah, _Logan’s Run_.
I took me imdb.com and _Soylent Green_ to find it back.
While doing so, I learnt that _Soylent Green_ happens next year, 2022. :-)
Great movie.. In the book, the age was 21..
Unfortunately, the actors were past that, so it was changed to 30 for the film.
Which isn’t so bad, actually.
People used to say life just starts at age 30..
https://en.wikipedia.org/wiki/Logan%27s_Run
Or 66, if we include that song.. :)
https://www.youtube.com/watch?v=4ay8C8dAqEg
Hmm… I can’t help but think that genetically modified pigs could be used as donors. It would make it easy to keep the blood alive because it’s just in the pig.
Normal pigs are already used as Doners, so why not?
My beef (!) with this article is the units! I really need to know how my fluid ounces there are, for my black pudding recipe.
Well if the grass munchers get their way, we can still save the pig species by using them as blood and organ donors.
That’s the problem with vegans, they want to make animals extinct by us not eating them.
So lets kill them and harvest their blood for other uses, even if black pudding is scrummy but we are not allowed it.
Oh yes, like all the ‘almost-extinct’ species around before humans saved them by munching on them. /rolls_eyes.gif
Your problematic line of thought supposes that animals with no utility to people must have no reason to exist; one of the reasons the world is in such terrible shape…
Mosquitos, cockroaches and viruses (non-autonomous ‘things’, but still) don’t have any business existing, no. The rest will be useful for biotechnology. And no, the reason the world is in a terrible shape is the monopolization of the economy in the hand of private actors that only care about profit.
When I was in high school chemistry class, the teacher gave a lesson about artificial blood being used in the Vietnam War (I’m American). It was made of coconut milk, because it loosely bound with the oxygen. I thought for sure that it would have been studied and improved on since then.
If I remember things correctly (allways suspect) there are a few key details different.
Coconut water, the clear juice inside coconuts, was used. Coconut milk is that juice mixed with coconut pulp; too chunky for blood. Coconut water happens to be pretty sterile, never being exposed to air, is pretty close to 0.9% saline (normal saline), and is around 5 to 10% dextrose.
That makes it a pretty close match to what is used in many hospitals.
That’s fluid volume, not oxygen transferring blood. It will allow a body to have enough blood pressure and hydration to allow the heart to pump (the remaining) blood and bloodcells around losing blood volume to an injury, but this liquid will not really be transferring oxygen like blood with blood cells does..
While not much good for improving storage requirements or infection control, an interesting avenue would be ‘genericising’ donated blood to avoid the type rejection issue. e.g. by adding molecules that bind to an antigen and express a different antigen and cleaning antibodies from donated plasma, effectively transforming effectively all donated blood cells to group O- and all plasma to group AB.
Ehh just use the boll from and andes area Humming bird.
Damn I mean Blood form a humming bird that live in the Andes mountains in South America.