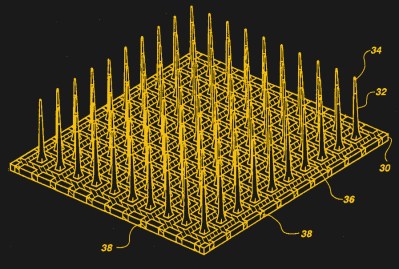
When we think of brain-computer interfaces (BCIs) that use electrodes, we usually think of Utah arrays that are placed directly on the brain during open brain surgery, or with thin electrodes spliced into the exposed brain as postulated by Neuralink. While Utah arrays and kin as a practical concept date back to the 1980s, a more recent concept called Stentrodes – for stent-electrode array – seeks to do away with the need for invasive brain surgery.
As the name suggests, this approach uses stents that are inserted via the blood vessels, where they are expanded and thus firmly placed inside a blood vessel inside the brain. Since each of these stents also features an electrode array, these can be used to record neural activity in nearby neural clusters, as well as induce activity through electrical stimulation.
Due to the fact that stents are already commonly used by themselves in the brain’s blood vessels, and the relatively benign nature of these electrode arrays, human trials have already been approved in 2018 by an ethics committee in Australia. Despite lingering concerns about the achievable resolution and performance of this approach, it may offer hope to millions of people suffering from paralysis and other conditions.
Using Existing Infrastructure
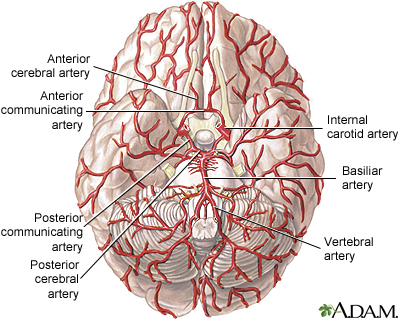
The human brain is of all the body’s organs the one that relies the most on a constant supply of oxygen and nutrients to function and survive, and thus has a very dense network of blood vessels that innervate every single part. While many of these blood vessels are too narrow for medical interventions such as a cerebrovascular stent, starting with the jugular arteries and veins, a large part of the brain’s vasculature is thus accessible.
In the case of a Stentrode, a similar approach is thus employed as with a regular stent, in that using a guidewire the device is guided into position via the jugular vein and external tracking to ensure it reaches the appropriate location prior to deployment. Over the course of a few weeks the stent anchors fully into the inside of the blood vessel, where it can remain virtually indefinitely to provide mechanical support or whatever other function is required.
While for the treatment of cerebrovascular conditions using stents there’s no question about why you’d want to use this approach – since the sole goal is to deploy the supporting stent inside the blood vessel – in the case of an electrode array that is supposed to interact with the brain’s neurons there’s the question of why you would want to choose this approach.
The obvious answer is that it involves non-invasive surgery, with no opening of the skull, and little risk of complications such as inflammation of the brain and other adverse affects that may result from invasive brain surgery. This makes it very different from the standard Utah (or microelectrode) array approach, as well as the electrode strings proposed by Neuralink. Theoretically Stentrodes could be placed under local anesthetic, with essentially zero recovery time afterwards required.
Although the benefits here are obvious, the questions that remain are how the performance of Stentrodes compares to other electrode arrays, and whether Stentrodes pose long-term risk in terms of blood clotting and similar cardiovascular issues, due to the necessity of having conductors running inside cerebral veins to conduct signals to and from the array.
Checking The Studies
The first research on these endovascular stent-electrode arrays was performed as far back as the 1970s (Penn et al., 1973), with Soldozy et al. (2020) providing a systematic literature review in the Journal of Neurosurgery. As noted by Bower et al. (2013), for traditional neural implants transcranial surgery is required, via a burr hole or craniotomy (lifting of part of the skull), which limits the attractiveness of the use of intracranial implants.
In the Bower et al. study, they compared intravascular electrodes with subdural electrodes, finding a similar recording response with induced epileptic activity for both. In the Opie et al. (2016) proof-of-concept study Stentrode implants were used to stimulate parts of a sheep’s motor cortex with a 4 mA -6 mA current.
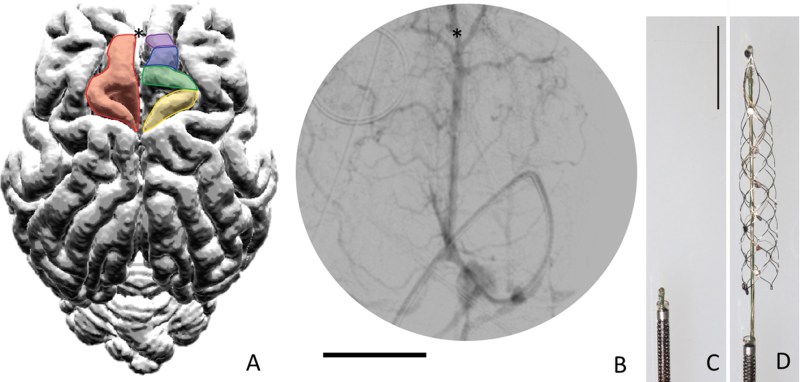
In a study with two sheep that had either just a Stentrode, or a Stentrode as well as a subdural and epidural array implant on either brain hemisphere, Forsyth et al. (2019) found that the accuracy of determining the sheep’s movement from the recorded data was as good if not better with just the Stentrode. Along with the results of e.g. John et al. (2019) that saw a similar study performed, this suggests that Stentrodes may be a viable BMI implant.
This then mostly leaves the question of the long-term implications of running wiring through these blood vessels, especially in terms of clotting and other, potentially fatal complications. In the meta-analysis the maximum study duration with live sheep subjects was 190 days. At the end of the study the sheep were euthanized and an autopsy was performed to assess the state of the implant.
The used devices were made out of Nitinol, which appears to have good biocompatibility and in-vivo is observed to induce neointimal coverage, which both stabilizes and anchors the material into the blood vessel’s wall. It is likely that this will also prevent the formation of blood clots, though long-term studies are required for a solid conclusion here.
Human Test Subjects

As noted earlier, the minimally invasive nature of a Stentrode implant and its adaptation of existing, approved medical devices and techniques have made its testing in human subjects. The company marketing the Stentrode, Synchron Medical, is currently running a clinical trial in a few locations in Australia. This study targets people who have suffered an injury or have a condition that prevents them from fully using their limbs.
Using what Synchron calls the Motor Neuroprosthesis these subjects are implanted with Stentrodes that will record the activity in their motor cortex and ultimately restore muscle control to the patient’s limbs. With the study only having started in June 2022 it will still take until the end of 2023 before the study is expected to deliver results on whether this is a viable treatment for people who suffer from paralysis, but who still have a functional motor cortex.
More details are provided on the Synchron website, which lists past, current and upcoming clinical trials. The clinical trial that just began follows the Switch 1 trial, which confirmed the biocompatibility of the device in a human subject. The Command clinical trial appears similar to the Switch 2 trial, but takes place in the USA . Trial subjects are implanted with the Stentrode device and a transceiver unit in the chest, with communication with the transceiver apparently occurring via Bluetooth.
No Silver Bullet
As with all brain-machine interfaces, it remains important to understand the limitations of current technology. One major aspect of most brain activity recording devices in use today and in clinical trials is that they are uni-directional. For example, they read activity in the motor cortex and use that data to interpret the intended action and perform the limb movement. Yet the sensory input from the body part being manipulated is not provided back to the patient’s sensory cortex, instead ending up petering out in the spinal cord or wherever else the discontinuity starts.
This is something which is also being addressed with current research, but the challenge remains to provide a robust interface between computer systems and the fickle nature of biological systems. Ideally we could provide a 1:1 mapping between the motor cortex and muscles, and back from the sensors to the parts of the brain which process touch and other sensory inputs, in order to restore full biological functionality.
What is however encouraging is to see multiple, different and perhaps complementary approaches being employed and developed. Even if we don’t have the perfect way yet to undo the ravages of injury and disease, with sustained effort we will find ways to address the remaining issues. Regardless of whether the best solution turns out to be fully electrical, regenerative therapies of the remaining tissues, or a combination thereof, it is the quality-of-life improvement that these therapies provide which make them so worth pursuing.













Ohhh Yeah Baby – Sign Me Up! I am losing soooo many brain cells these days due to never-ending YouTube butt-in ads (ouch), maybe this can help??
No, but you may be able to play flappy bird without a keyboard.
I just love the combo of uBlock+SponsorBlock under firefox. It’s so awesome that some of the videos from LTT become somehow bearable :D
I try to NOT use ad blockers, Often the per session retaliation against ad blockers is worse than the cure. I WANT content providers I visit regularly to earn money from ads that may interest me. I do NOT want Google/YouTube to feed me anything based on their WRONG assumptions built-up over time by spying on me. All my online browser ad blocker add-ins are carefully managed by me in real time. BTW do you know your Firefox browser is always allowing Google to spy on you – for money?
Oh you think they won’t put advertising in your brain? Hahaha
This procedure may be able to save many politicians from needing to undergo complete cranial crapectomies!
For that, you’d also need a catheter.
By “uni-directional” that means basically RS232?
It means “don’t freak out about this while we quietly work on making them bi-directional.”
Boy, I can’t wait until I can be switched off like a toaster.
As long as the aging process is suspended when “off”, and complete reactivation is guaranteed!
These comments got _dark_!
You’re welcome 😊
The implications of wirehead tech inevitably do—you can’t really escape them.
Sorry Elliot – not everyone in here likes the idea of being cattl..ahem carefree as much as you do 😁
Any procedure that goes through blood vessels like this is crazy dangerous, they do it for heart surgery because the alternative is litteraly death. Poke in the wrong place and vessels can spasm and you die, plen of people die during “routine” angiograms
And what is the failure mode like when your body experiences high jerk, or jolt (rate of change of acceleration). e.g. falling down, elevators stopping, in any vehicle that crashes.
The science of splashmatics.
Uhm… Isn’t it technically invasive. Non-invasive would normally imply getting brain signals externally, by placing electrodes on skin (on limbs or on chest for specific signals or on crown region for moar signals), or by using brainwaves (not technically the signals themselves, but the noise spectrum of the signals), or MRI (again not the signals themselves, but the locality and intensity of the brain activities). Even an actually invasive electrode placement in the limbs would be much less invasive.
All for progress of technology but there are of course problems to solve with this approach. Any indwelling device like this will likely require anti coagulation so clots don’t form exactly where the device is and presumably where cut off blood flow would be the worst. The brain is unique (surprise)in that a lot a it’s blood supply is via what are called terminal arteries, meaning there is no collateral blood flow if one supply is cut off. This is very different than most other body systems. Systemic anti coagulation is also an advance but has tons of potentially fatal problems as well. And I agree that the jargon “minimally invasive” is a bit misleading. Just because you avoid a craniotomy you are still leaving a foreign body deep in the brain. We also do awake craniotomy under light sedation so while a “crani” isn’t exactly benign, we can’t even do an appendectomy without general anestheisa. All stuff to think about.
Can’t wait to try it out.. though, I have a hard time finding volunteers.. especially, since last time I did medical equipment and a prototype lit up like a flash and disappeared… but hey, I was just an ear probe… told my boss, that the current needed for that measuring system was way off..
I’ll start on a hobby project using it as soon as I find a new volunteer…
You’ll be surprised. Some promises of “safety” despite a lack of long term data, a bit of censorship, some coercive measures, restrictions of civil liberties, a promise of return to normal if you just have the procedure. And voila, popular buy in.
Never underestimate to power of propaganda. Did I say propaganda, I meant marketing.
That could never happen. Medical ‘professionals’ and ‘scientists’ wouldn’t allow it and the media would expose it. Certainly sites like this would be invaluable in combating that type of marketing.
;D This!