The brain is a rather important organ, and as such, nature has gone to great lengths to protect it. The skull provides physical protection against knocks and bumps, but there’s a lesser-known defense mechanism at work too: the blood-brain barrier. It’s responsible for keeping all the nasty stuff – like bacteria, viruses, and weird chemicals – from messing up your head.
The blood-brain barrier effectively acts as a filter between the body’s circulatory system and the brain. However, it also frustrates efforts to deliver drugs directly to the brain for treating conditions like brain tumors. Now, scientists have developed a new technique that may allow critical life saving drugs to get through the barrier with the help of ultrasound technology.
A Protective Barrier
The blood-brain barrier is a complex network of blood vessels and cells, effectively acting as a filter between the body’s circulatory system and the brain. It’s incredibly effective at its job, allowing only specific substances to pass through and reach the brain while keeping out potential toxins or pathogens. This barrier is vital for maintaining the brain’s stable environment, crucial for its normal functioning.
First discovered in the late 19th century, the barrier was revealed when German physician Paul Ehrlich noted that dye injected into a mouse’s bloodstream did not reach the mouse’s brain or spinal cord. It would take a further century or so for technology to advance enough to reveal more about the barrier’s physical characteristics.
The key to the barrier is a structure created by endothelial cells. These cells can be found lining all blood vessels, but in the blood-brain barrier, they are altogether wedged together much closer in what are called “tight junctions”. They essentially create a sort of sieve that is only fine enough to allow small molecules, fat-soluble molecules, or certain gases to pass through. Other larger molecules, like glucose, can only gain entry through special transporter proteins that carry them through the barrier.
A New Approach to an Old Problem
However, this highly specialized security system presents a significant obstacle when it comes to treating brain diseases, particularly cancers such as glioblastoma. Glioblastoma is a particularly aggressive and deadly form of brain cancer, and existing treatments often prove ineffective. One of the key reasons for this is the blood brain barrier, which prevents many chemotherapeutic drugs from reaching the brain, rendering them largely useless for this type of cancer.
In this realm, a team of researchers from Northwestern University has made a breakthrough. They’ve leveraged the power of ultrasound, to make the blood-brain barrier temporarily permeable. This allows crucial drugs to reach the brain to treat glioblastoma without permanently compromising the barrier and thus the patients health.
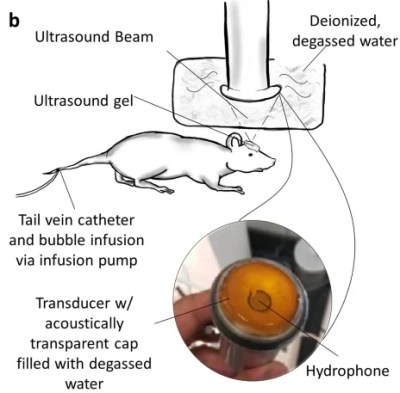
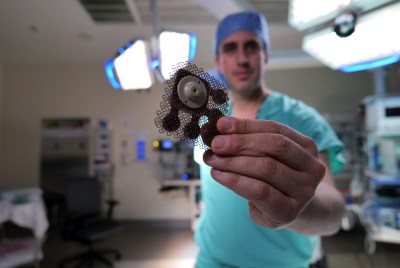
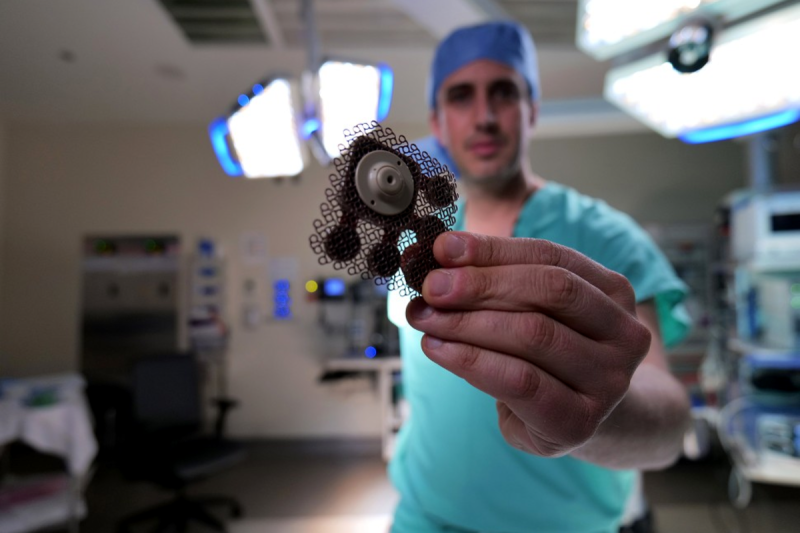
The technique involves fitting the patient with a skull-implantable ultrasound device. The ultrasound device generates sound waves that interact with injected gas microbubbles which allow the blood-brain barrier to be temporarily opened.. The procedure takes approximately four minutes, and is performed with the patients awake and conscious. Opening the barrier in this manner allows powerful chemotherapy drugs like paclitaxel and carboplatin to pass through into the brain.
Using microbubbles to permeate the barrier has been the subject of research for over a decade, and is only just reaching clinical application through trials like the one conducted by Northwestern University. The technique is referred to as microbubble-assisted focused ultrasound blood-brain barrier disruption, or MB+FUS BBBD. It’s believed that fluid effects resulting from the cavitation of ultrasound-induced microbubbles are what helps permeate the barrier. However, the specific mechanism of action is difficult to tease out due to the difficulty, or impossibility, of directly observing microbubble activity in the brain’s vasculature.
In a first-of-its-kind human clinical trial, this technique has been used to deliver chemotherapy to large, critical regions of the brain affected by glioblastoma. The ultrasound device was able to repeatedly open the BBB, demonstrating the potential for ongoing treatment strategies. Success of the procedure was measured by using fluorescent dyes to measure permeation through the blood-brain barrier, as well as MRI scans performed after the ultrasound activation. Researchers found that the barrier was mostly closed around 1 hour after treatment. Previous studies suggested full restoration of the barrier after 24 hours; this latest work suggests the time scale may be much shorter.
Importantly, the research also noted the benefits of the ultrasound implant used in the study. Early research used a single ultrasound emitter, while this latest study used an array of nine emitters in an implantable grid. This enabled a far wider swathe of the blood-brain barrier to be opened up, allowing drugs to more effectively reach the broader volume of the brain.
More To Come
This innovative use of ultrasound represents a potential game-changer in the treatment of glioblastoma. By bypassing the blood-brain barrier, previously ineffective yet potent chemotherapy drugs can now reach the brain tumor, providing new hope for patients.
This novel technique’s potential reaches beyond the realm of glioblastoma treatment. The ability to permeate the blood-brain barrier and deliver therapeutics directly to the brain could open new avenues for treating a wide array of neurological disorders. Diseases such as Alzheimer’s, Parkinson’s, and other neurodegenerative conditions, where the blood-brain barrier has historically impeded drug delivery, could potentially benefit from this technology.
While further research is undoubtedly necessary, this breakthrough signifies a critical step forward in neurology and oncology. It provides a promising glimpse into the future of brain disease treatment, where overcoming the blood-brain barrier might become a standard procedure. As the field of medical technology continues to evolve, developments like these represent monumental strides towards transforming patient care and improving health outcomes worldwide.














Ahhh “drug delivery” and “cancer research,” source of infinite grants and zero usable products. Thanks for getting so many PhDs their daily bread
You may think the success rate is low and then what is the point throwing all the money at it for little benefit, but when there is a success then benefit is overwhelming.
People play lotteries with pathetic rates of return, but just occasionally someone gets lucky.
The point is, the overall success rate isn’t important per se, but that the success is so great when it happens that it’s worth the investment.
You are clueless. As one who has survived an incurable cancer for >14 years and seeing how hard the oncology community works to get results, it is more than obvious to me than you are uneducated.
You took that a bit personal, so your answer is clearly also disqualified.
This is simply not the case. Cancer research pays dividends in understanding constantly. Does it always result in treatments for the specific cancer they are researching? No, but it is because this stuff is hard.
@TG
You can only be so cynical if you know no one having survived cancer 10 years ago.
I don’t wish that experience to you.
This.
“The brain is a rather important organ…” and yet so many people seem to get through life without one.
I do wonder though what the long term effects of using ultrasonics and bubbles to “wedge” open the blood brain barrier would be? (Make it more permeable, less permeable, who knows?)
Indeed, assuming it has any lasting effect at all. Which they seem to think it won’t, almost back to normal in an hour, entirely in a day or so it seems. Though either way if you have something like cancer that is killing you NOW potential further problems LATER are still worth the risk – where there is life there is hope.
Hi, There are no consideration of long term effect cause by a treatment of glyoblastoma. Médium survive is few years after diagnosis.
I understand that the potential long term effects compared to the ability to treat a cancer make it a no brainer (no pun intended) for treatment, but if it is successful then it will probably be applied to other diseases. It sounds promising, just want to know the long term effects if it’s applied more broadly.
Just remember to examine risks in context. E.g. (pick an arbitrary number) a 0.1% risk of eventual disability from a treatment that cured cancer would be a huge benefit for most cancers (injured beats dying), but unacceptable in a treatment for broken arms.
This is a major reason new treatments may first be available only to the terminally ill: they have the greatest need, and are the most likely to get more good than harm, if the treatments unexpectedly turn out to cause harm or have delayed effects.
There are processes in place to watch for long-term risks for new medications and treatments. Guaranteed more good than harm is standard.
In fact there’s the opposite question: whether (and how much and how many) beneficial treatments are delayed and discouraged by all the precautions. Resulting in lost lives and health that could have been saved but were not, due to excessive precautions.
Here, if there’s no known long-term risk — just people wondering “what if” (and it’s trivially easy to say “what if”) — I would just want to be sure appropriate testing would be done for the intended usage. Having been involved in medical software development, appropriate testing is definitely done.
I’m curious what frequencies were used in the study.
The previous single-emitter version (Sonocloud-1) used 1 MHz, at modest intensities.
The frequencies and intensities used here are within the range of ultrasound already used transcranially, through the intact skull. It’s not clear why they would need to cut open a chunk of the skull just to install the ultrasound transducer. It’s easy to get a substantial amount of ultrasound power into the brain even through the skull. It’s been easy for more than forty years.
And I’m curious what words I used in my reply that caused it to go into the mod queue.
“My brain? That’s my second favorite organ.” –Woody Allen (Yes, I know he’s not an exemplary human being, but the line is very funny)
This was also done in the Netherlands a year ago.
https://www.umcutrecht.nl/en/over-ons/nieuws/brain-center/opening-the-blood-brain-barrier-with-sound-waves
This technic exist (at least) since 2016 : (in french) https://presse.inserm.fr/tumeurs-cerebrales-pour-la-1ere-fois-des-ultrasons-rendent-permeables-les-vaisseaux-sanguins-pour-accroitre-la-diffusion-du-traitement/24277/
It’s the “blood/brain” barrier. What is a blood-brain? The center of consciousness for blood?