By and large, the human body is designed to breathe from birth, and keep breathing continuously until death. Indeed, if breathing stops, lifespan trends relatively rapidly towards zero. There’s a whole chunk of the brain and nervous system dedicated towards ensuring oxygen keeps flowing in and carbon dioxide keeps flowing out.
Unfortunately, the best laid plans of our body often go awry. Obstructive sleep apnea is a condition in which a person’s airways become blocked by the movement of soft tissues in the throat, preventing the individual from breathing. It’s a mechanical problem that also has a mechanical solution—the CPAP machine.
Under Pressure
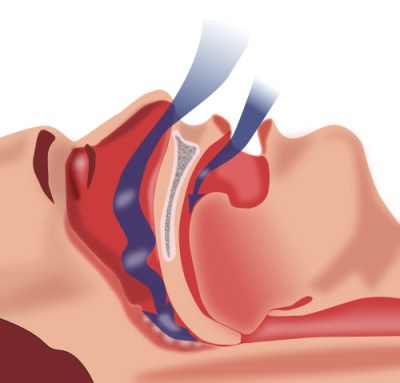
The underlying mechanism of obstructive sleep apnea (OSA) is quite straightforward. During sleep, as the throat, neck, and skeletal muscles all relax, the tongue and/or soft palette can come to block the airway. When this happens, fresh air cannot pass to the lungs, nor can the individual exhale. Breathing is effectively halted, sometimes for minutes at a time. As the individual’s oxygen saturation drops and carbon dioxide levels build up, the brain and nervous system typically trigger an arousal in which the person enters a lighter stage of sleep or wakes up to some degree. The arousal may simply involve a change of position to restore normal breathing, or the individual may wake more fully while gasping for air. Having cleared the airway and resumed normal respiration, the individual generally returns to deeper sleep. As they do, and the muscles relax again, a further obstructive apnea may occur with similar results.
For those suffering from sleep apnea, these arousals can occur many hundreds of times a night. Each disrupts the normal cycles of sleep, generally leading to symptoms of serious sleep deprivation. These arousals often occur without the individual having any awareness they occurred. Sleep apnea can thus easily go undiagnosed, as individuals do not know the cause of their fatigue. In many cases, reports of heavy snoring from sleeping partners are what leads to a sleep apnea diagnosis, as breathing typically becomes louder as the airway slowly closes due to the muscles relaxing during sleep.
Ultimately, the solution to sleep apnea is to stop the airway becoming blocked in the first place, allowing normal breathing to continue all the way through sleep. The problem is that it’s difficult to access the tissues deep in the airway. One might imagine placing some kind of mechanical device into the throat to keep the airway open, but this would be highly invasive. It would also likely pose a choking risk if disrupted during sleep.

Enter the CPAP machine—short for “continuous positive airway pressure.” Invented by Australian doctor Colin Sullivan in 1980, the idea behind it is simple—pressurize the individual’s airway in order to hold it open and prevent the tongue and soft tissues from causing a blockage. Air pressures used are relatively low. Machines typically deliver in the range of 4 to 20 cm H2O, which has been found sufficient to keep an airway open during sleep. The CPAP machine doesn’t breathe for the user—it just provides air to the airway at greater than atmospheric pressure.

Key to the use of CPAP is how to get the pressurized air inside the airway. Early machines pressurized a large helmet, with an air seal around the neck. Today, modern CPAP machines deliver carefully-controlled pressurized air via a mask. Nasal masks are the least-invasive option, which pressurize the whole airway via the nostrils alone. These masks require that the mouth remain closed during sleep, else the pressurized air is free to leave the airway. Full-face masks, which are similar to those used for other medical procedures, can be used for individuals who need to breathe through their mouth while sleeping.
Overall, a CPAP machine is relatively simple to understand. It consists of a pump to provide pressurized air to the mask, and a user interface for configuring the pressure and other settings. CPAP machines often also feature humidification to stop the supplied air from drying out the user’s mouth and/or nose. This can be paired with heated tubing to warm the air, which avoids condensation from forming in the tube or mask during use. This is called “rainout” and can be unpleasant for the user. Modern machines can also carefully monitor pressure levels and airflow, logging breathing events and other data for later analysis.

CPAP treatment is not without its issues, however. Users must grow accustomed to wearing a mask while sleeping, as well as adjust to the feeling of breathing in and exhaling out against the continuous incoming pressure from the machine. It’s also important for users to get a suitable mask fit, to avoid issues like skin redness or pressure leaking from the mask. In the latter case, a CPAP machine will be ineffective at keeping an airway open if pressure is lost via leaks. These problems lead to relatively low compliance with CPAP use among those with obstructive sleep apnea. Studies suggest 8% to 15% abandon CPAP use after a single night, while 50% stop using CPAP within their first year. Regardless, the benefits of CPAP machines are well-supported by the available scientific literature. Studies have shown that use of CPAP treatment can reduce sleepiness, blood pressure, and the prevalence of motor vehicle crashes in those with obstructive sleep apnea.
Nobody likes the idea of being semi-woken tens or hundreds of times a night, but for sleep apnea sufferers, that’s precisely what can happen. The CPAP machine is the mechanical solution that provides a good night’s rest, all thanks to a little pressurized air.
Featured image: “wide variety of masks at cpap centra” by [Rachel Tayse]. (Gotta love that title!)













I’ve been using mine for more than 25 years, and it’s been a great help. Before I was diagnosed with apnea, I was passing out while driving in the middle of the day despite doing everything I could to keep myself awake. By the time I had been using CPAP for a month, I had stopped passing out behind the wheel completely.
A coworker had 3 car accidents that could be attributed to this; he was prescribed a cpap machine and never used.
The medication he was on gave him tremors which later became permanent. He was put on leave multiple times for falling asleep in meetings at work; and was eventually pushed into retirement.
He walks with a cane now, and needs help to do things like buy groceries.
This is what happens when you try and fix the problem without addressing the underlying issues.
Are there any novel alternatives? Sleeping with a mask on sucks.
There’s an implant. Don’t know much more than that, but it seems geared towards light snorers.
Daily exercise. Different bed and pillow. Cooler sleeping conditions. O2 generator with a nasal cannula.
Exercise only helps in some few cases. Most apnea patients have airway constrictions that have nothing to do with being overweight.
Sleep position has an influence on apnea severity. Sleeping on your back is the worst position. It makes apnea far worse. Better is to sleep on your side, with a pillow that is high enough that your wind pipe is straight.
I don’t know that cooler is better, but from the temperatures the last few weeks it seems that warmer is worse.
There are some people who need oxygen in addition to CPAP because they have other lung problems. Oxygen alone doesn’t do the trick. It doesn’t matter how much oxygen is in the air if it can’t get to your lungs.
The science disagrees with you. It’s a convenient line for the body positivity movement but weight loss is a potent treatment in many cases.
https://doi.org/10.1378/chest.09-0360
Skinny guy here with (former) sleep apnea. There are multiple causes of sleep apnea. Most, however, are probably associated with being somewhat overweight, just not all. I had to get surgery (turbinate reduction) after 8 years of using CPAP. Thank goodness it helped.
I wish there was more innovation on CPAP masks. They work (trust me) but they do suck to use.
Wearing a mask and not sleeping didn’t feel so great. For the month I tried CPAP, I didn’t sleep more than 4 hours per night. That was considerably less than I got with my disturbed sleep. It did not progressively get better, despite 100% compliance.
I sure wish it had worked. A surgical fix (cause=abnormal tissue formation/amount, not a weight issue) sounds quite miserable.
I know somebody who has the Aspire implant. Last I heard, he had abandoned it.
There are jaw positioning devices that have helped some people I know, but not me. Expensive for what they are, but worth looking into.
Don’t know if it’s encouraging or not, but it took more than a month for me to be used to the CPAP. It also kept me awake. It might help to alternate between using it and, it did help me getting used to it. Still sucks to use it though. :-/
Also, only the full mask ever worked for me.
Agreed…The best solution I found is the full face mask F20 with memory foam surround on my AirSense 10. Sounds a bit over-kill but I reliably sleep for 7 hours with the mask on now. BTW, I also 3D printed some supports for the tube that suspends it over the bed. Still, there are some nights I rip it off of my head :-/
For the jaw positioning device, if it’s what we call “Orthèse d’Avancé Mandibulaire” here, then, it indeed work.
But it’s a timed solution, your teeth will eventually move, both making them misaligned (I had to change the way I bite and chew), and rendering the device inoperative.
It’s not expensive tho, hundred(s) of dollars I think (it’s covered by health insurance here).
Technically, it’s just an overmolding of your teeth with two adjusted lever to force your jaw forward.
It helped me greatly when it worked, but now, almost a decade later, it didn’t work anymore and started to cause teeth pain, so I stopped it.
I wish you to heal, it’s not a funny disease.
For some a MRA will work. A bit over your teeth. And for some operations. Contact a specialist. Sleeping with a mask is a small price to pay to get your life back. It will give you your energy back.
Lose weight, stop drinking, don’t sleep facing the ceiling. But mostly lose weight and stop drinking. Just about everyone these days needs to lose some weight and also reduce stuff like tissue inflammation that really exacerbates this.
Losing weight only helps in a small percentage of cases. Most people with apnea simply have narrow airways.
Alcohol causes your muscles to relax, which can make apnea worse. Not drinking reduces apnea a bit, but will not make it go away.
Eh I think a much broader set of cases is related to being overweight than we are admitting right now. Most body types we now consider as normal would have been classed as overweight only a few decades ago, and most people who think of themselves as in shape or even skinny are deluding themselves
I was 5′ 10″ (1.8 meters) and weighed 135 pounds (62 kg) when my wife noticed that I had apnea. I don’t think that counts as overweight.
“Here is a general statement about an aggregate population”
“Oh yeah well I know a guy who is an exception, so the average doesn’t exist”
You failed, sorry about your sleep apnea though
People love to recommend losing weight as an alternative to using a CPAP, but often weight gain is related to poor sleep. Unreasonable working hours and at times maintaining multiple jobs/side-hustles limit people’s ability to go out during the day, exercise, meal prep and eat properly, etc…
All of those things affect sleep quality in addition to overall health, which leads people to gain weight. Even if weight gain is the cause of sleep apnea, and it’s usually a combination of factors, untreated sleep apnea can make losing/managing weight impossible.
I felt like absolute shit when I started using a CPAP and I slept worse for the first month. Then I adjusted to it and immediately started having more energy to exercise, fewer horrible cravings and drops in energy, I healed quicker, I got sick less, all made it easier to exercise and eat correctly and I ended up almost effortlessly dropping 70lb. Now I am much healthier and have fewer apneic events, but I still use my CPAP because I still stop breathing in my sleep without it even when I am at a healthy weight since losing weight didn’t magically change the shape of the inside of my face, cure my allergies, etc…
Pretty fascinating angle on it, I’m certainly glad to entertain the idea that the causality is reversed.
Same thing for me, I changed doctors and he had exactly the same reasoning about the fact that I couldn’t control my weight.
I went to see him for increasingly frequent problems where I woke up in the middle of the night with the airways blocked, before that rarely happened to me, like when I had a cold, but it started to do it to me any night. He told me that it is surely due to a severe apnea and prescribed me one night with a ventilatory polygraph. Result: 40-something sleep apnea per hour.
So prescription of a CPAP and there he asks me if I’m having trouble losing weight, I explain to him that it’s the yo-yo, by making consistent efforts I manage to lose well but impossible to stabilize. And there I heard the same speech, so that people don’t realize how much of a vicious circle it is, that losing weight helps to fight sleep apnea, but that sleep apnea can also cause rapid weight gain. As well as the migraines, which I had every week…
It took me about 4 weeks to adapt, but what a crazy sensation it was to wake up in the morning without being tired, I didn’t even realize how exhausted I was.
The migraines are still there, but much more spaced, sometimes months.
And in 3 years I lost almost 20kg, it’s not just apnea that is responsible, but I think it played a great role in the balance.
Superconducting magnets that reduce the gravity on tissues (like the classic levitating frog experiment) ;)
An alternative is an “Oral Appliance”, of which there are two major types.
Mandibular Advacement Devices (MADs) which are like a night guard/retainer for both the top and bottom teeth. The bottom is adjustable so you can pull forward the lower jaw by a few mm and unblock your obstructed airway as a result. This can cause jaw soreness and bite issues in some patients, and you typically need to do some jaw stretches before and after sleep to prevent that, and to keep your lower jaw from “learning” that forward-biased position (resulting in the patient developing an underbite).
Tongue Stabilizing Devices (TSDs) use a suction bulb to pull the tongue forward, which also helps prevent the airway from becoming obstructed. These are usually only prescribed to people who’s teeth aren’t strong or numerous enough to use an MAD.
Oral appliances don’t work for all apnea cases, especially with more extreme obstructions, so a CPAP is necessary for some patients. My Fiancé uses an MAD and it works excellently for her case. It is cheaper, more convenient, and more sanitary than a CPAP.
Further reading: https://my.clevelandclinic.org/health/treatments/21129-oral-appliance-therapy-for-sleep-apnea
Tbf, that part is subjective.
For me and a few other folks I’ve met, the mask becomes part of the bedtime routine and helps tell the brain that it’s sleep time. I used to have a lot of trouble falling asleep, but now I just put the mask on and my brain shuts off.
It’s also adds some minor conveniences, like the humidifier (so you don’t have to humidify the whole room and risk mold) and the fact that you can completely cover yourself in blankets and still breathe. The modern machines are also freakishly quiet.
Airlines legally can’t charge you extra to take the machine on flights (in the US, at least), and car camping still works fine with big ol’ battery. Backpacking is probably the one thing that gets a lot more difficult.
It definitely sucks a lot for some people though.
Agreed. Had one for a few months. Couldn’t sleep with it and I ended up worse than I had begun. Ended up having nasal surgery and losing a bunch of weight and the problem was resolved.
I’m an old MD & ex-Pilot who had this issue & was forced to use CPAP for years by the FAA.
Other treatments are nasal airway, “LAUP” operation, plus some intra-oral devices may help.
I solved mine by losing 68#.
Take up playing the didgeridoo: https://pmc.ncbi.nlm.nih.gov/articles/PMC1360393/
Reading helps me fall asleep
It varies!
One path to this is that the core jaw muscle can loosen during sleep and the tongue presses back against the airpath. The solution to this can be a jaw jig (think a retainer or mouth guard) that tugs the lower jaw forward and keeps your airway clear. Insurance can make it easier but they’re $$$
Another option is a Bipap — CPAP is one way, BIPAP sucks on the exhale and matches your breathing back and forth. By adding some pressure forward, it’s attempting to overcome the muscular obstruction. CPAP has a bit of a survivorship bias issue, and people who talk about BiPAPs often get overshadowed by the (very successful!) folks who have had their lives changed by a cpap machine. If you’re currently using a CPAP, talk to your sleep doc about trialing a bipap.
There are surgical interventions that aim to help, but they’re expensive and low efficacy in general.
There are a couple of options that use a modified pacemaker to keep the muscles under a little bit of tension during inhalation, which is an option if you’re willing to use an implant.
All in all, there’s no one-size-fits-all solution but we’re getting closer.
No mention of the sound-deadening PE-PUR foam that has been silently degrading in these machines for years, filling user’s lungs with carcinogenic by-products? Nothing about how many owners are still unaware their machines had been re-called, or that manufacturer’s had suspiciously ceased operations?
The Phillips machines, but the Resmed 10s, 11s and Air Minis are clean, I think.
Only specific models of Philips machines. It is not just CPAP machines, though. There were all kinds of breathing assistance devices affected:
https://www.usa.philips.com/healthcare/e/sleep/communications/src-update
If I skip using mine for more than a single night, I get horrible headaches. Still, I struggled with building the habits of emptying the water reservoir in the morning, filling it at night, and putting the mask on at the appropriate time. I fell asleep with everything ready to go, but the mask off, a lot in the early months.
I wanted to build some sort of “You’re not using it!” alarm, but I also didn’t want to touch the airway at all. I’ve seen a project that checked for air pressure differential between the airway and the room, but between “this is what keeps me breathing, a life-critical process” and the thought of spending all night breathing in microplastics from a 3D print (don’t get me wrong, I love 3D printing useful stuff), I just couldn’t do that. I tried monitoring the power usage, but using an appropriate current shunt for the maximum the power adapter could provide, I couldn’t get enough resolution to reliably see what little the CPAP drew when running. Plus it phones home and that was indistinguishable from running.
In the end, I created a custom bracket that mounted with some of the CPAP’s existing case screws, and held a micro-switch that detected when the humidifier reservoir was installed (with no modifications to the device). Then I changed my night routine to only insert the reservoir once I was ready for bed. The switch was connected to an ESPHome node of Home Assistant, and engages some colored LEDs elsewhere in the room to warn me that I need to take action. Flashing yellow at full intensity to empty it, or solid red at half intensity to remind me that I haven’t gone to bed yet. By this point I had enough of a routine that I very rarely needed an actual alarm for “you’re not using it,” but with Home Assistant that wouldn’t be a difficult feature to implement.
At my last annual checkup, my doctor told me I had 100% usage. The first year was very rocky, so hearing this was wonderful. Having a literal light glaring in the corner of my eye as bed time slowly approached was a big help for me.
Your clothes are shedding microplastics constantly and you are breathing them in.
I mostly wear cotton and linen. OK, sure, cellulose is technically a polymer but even vegans eat it :-)
I’d like to mention that for resmed 10 devices you can reflash the firmware quite easily to go from cpap to bipap to apap versions.
And also there are versions out there fully open up the pressure range, optionally disable the backup rate for those with UARS – check CPAPSupport subreddit.
It’s quite fascinating looking at the different algorithms these devices use and the difference between manufacturers.
Not a doctor, but diagnosed with sleep apnea in 2007. It literally saved my life. I agree that PAP is annoying and inconvenient, but for those of us who cannot get surgery (when the ENT says “major facial reconstruction”), it’s our best bet.
Posting to point out that in addition to obstructive there is also “central” apnea. Basically, for whatever reason your body just stops breathing. Many people have this, and for most it’s not an issue.
When you have both obstructive and central, that is called “complex” and that is where things get real fun. This is where one gets prescribed the $10,000 ASV machine.
There is a large population of non drinking skinny people with central OSA. They are hard to convince that their problems are sleep related but the couple of times they tried a cpap machine they all say “it saved my life”
My apnea is so bad I have to use a BiPAP, which detects when I am exhaling and drops the air pressure down low enough to allow me to breathe out. I believe it not only senses you breathing rate, but then predicts it a bit, as I cannot feel the pressure dropping or raising at all, but if I breathe quickly out of rhythm for a second I can feel the pressure change.
Also, some of them offer masks that cover the mouth and nasal passages, but don’t go over the top of the nose, leaving it clear to be itched. Might seem like a small thing, but it made wearing the thing every night so much more comfortable.
Life-changing little device though, for sure.
Been using one for years. Got used to it pretty quick. Definitely better sleep as a result.
Yeah, weight loss may help, but at my age weight loss is a difficult task. I’m slowly getting the weight down, but if you think it’s simple, you’re nuts.
Interesting tangent on ResMed. Likely applies to all off them though.
I helped my mother set one of these up years ago, and I was surprised to find a SIM card in it.
None of the paperwork had any mention of data collection or anything at all about ‘privacy’ related stuff.
So I popped the SIM out and the cell connection symbol on the UI changed to indicate ‘no connection ‘.
Perfect right?
Nope.
The machine powered on just fine but it reused to enter the actual sleeping mode.
It just threw an error saying it was unable to connect to the service.
After doing more research, there was no way to opt out.
And since the company classifies the data as “biometric” instead of “medical” data, they don’t have to comply with HIPAA.
And just in case there was even the slightest doubt that they were selling the data, it took less than 2 weeks for me to start getting cold-calls and internet ads about CPAP machines or services.
(And no, I did not use any of my accounts or phones while searching for info about that device or an opt out.)
I just love how being cyber stalked by dozens or for-profit organizations/corporations has become so completely normalized…
Yes, there’s a cellular modem in each machine. Always phoning home. Hell probably a microphone “snore sensor” and GPS receiver too. I’m sure the company has some clever ways to build up a user profile even if you don’t install the app, don’t create an account, and don’t register the machine…
Some do some dont.
You can still buy ones that do not have the sim.
What do you mean “buy”?
In just about every country these are classified as a “medical device” and require a prescription AND ongoing physician supervision.
I couldn’t find a single company that could legally sell one to me, that was WILLING to sell one to me directly.
You get whatever ones your doctor has, because those are the ones they have ongoing accounts with and the insurance process worked out for.
As we keep learning from examples like hearing aids, anything in the realm of “medical devices” is going to be HYPER regulated.
Sometimes it’s good.
Sometimes it’s not.
Bouhht both of mine without prescription “on the street”. They have odometers so you can check thrme hours.
Neither of mine have sim cards, and work fine.
The resmed cpaps can also be set to airplane mode to disable the cell connection. The UI constantly asks to re-enable the cell connection, but it’s not necessary. Frustrating that their unit creates a cellular company wifi access point when it is enabled. 😡
Free wifi?
The greatest hack is tissue inflammation from the things we eat. Alcohol, seed oils, gluten and poor nutrition in general. Coupled with how our sinus and mouth opening have reduced because of processed food is low crunch. Suggest fasting to give the body a break while using CPAP. sinus massage might help.
A better suggestion is not to give out quack “medical” advice on the internet.
You have no idea what you are talking about, so please stop.
It is ok you think this way. Food is medicine and the zip code you live in also dictates your outcome. When a person gets into a difficult spot like apnea their ability to troubleshoot and make changes is limited. Thus a doctor is needed. That is why prevention and making practical changes at first trouble is effective.
i am convinved that the high failure / abandonment rate of CPAP machines is due to consumer models being too basic a design. the next stage would be to have them read your inhalations & and exhalations and adjust the air flow, as opposed to continually forcing air down your windpipe all night long. it would make for a more peaceful sleep and an overall willingness to adopt the machine. i swapped out for a newer model that eases in to the full wind tunnel push after 45 minutes but i just end up throw the %$!&@* mask across the room a bit later than when i used the earlier model.
Modern machines do exactly that. On ResMed machines, it is called expiratory pressure relief (EPR.) Other manufacturers have similar functions under other names.
Say you have a pressure of 12 and an EPR of 3. That means that on inhale, you have a pressure of 12 and on exhale you have a pressure of 9. That’s pretty much what you wanted – lower exhale pressure to make it easier to breathe.
The problem is that reducing the pressure on exhale allows more apneas to happen. To make up for that, you have to raise the pressure, usually by as much as the EPR.
To make up for using EPR, you have to set the pressure to 15 to fix the apneas causing by reduced exhale pressure. That means an exhale pressure of 12, which is what you’d have had if you just turned EPR off.
Adding to that is the fact that the machines get out of step with your breathing when doing EPR or whatever your machine manufacturer calls it. There’s nothing quite like the joy of having the pressure drop to exhale while you are still inhaling.
I keep the EPR equivalent on my Löwenstein machine turned off. It has never done anything good for me, and has caused me many nights of grief before I figured out what was going on.
My pressure is at the higher end. 17-20 cmH2O. I have no trouble inhaling or exhaling. Put the mask on, breathe normally.
If you feel a “wind tunnel” in your face, then your mask is leaking too much, At my full pressure, I don’t feel any air flow on my face or in my mouth/windpipe.
Not only do they do exactly what you describe, and have done so for more than a decade, but they do more.
Even the cheaper machines now also ramp up from nothing to their operating pressures over time, so you start sleeping without feeling pressure (with adjustable ramps).
Most also have live adjustment that changes based on breathing patterns based on a best-guess on what type of sleep you are in, and not simply inhale/ramp-up vs exhale/cutoff.
It’s all jut simple sensors and software.
IMO the bigger problem with uptake is people being big babies that are unwilling to tolerate the slightest discomfort, regardless of the short/long term benefits.
Boo hoo. This thing is EVER so slightly uncomfortable!
Instead of adjusting to it until I don’t notice it anymore, I’ll just quit.
Future me will have to deal with the consequences.
Humans are all lazy, greedy, infantile goblins.
Sometimes those urges work out well, like when it drives us to create tools to make tasks easier or methods/processes to get better results.
But most of the time it’s a bad thing and requires active correction.
Thank you H.A.D. editor Lewin Day for the excellent description of the sleep apnea problem and CPAP machine solution. Yours was considerably better than the one given to me by my sleep specialist doctor and the equipment provider.
This being H.A.D. I’m surprised to see no mention of hacking these machines. I no longer use one (due to a dispute with my equipment provider and insurance) and cannot even remember the manufacturer name (one of the large medical equipment companies) but the unit contained wireless data circuitry to report daily results as soon as I turned off the machine. It may have used AT&T.
I was not fond of that privacy intrusion and was unable to apply the “38 caliber solution” to it because it was a rental. I tried wrapping the PCB in aluminum foil to no effect and gave up. Next step would have been to sleep in a Faraday cage :-)
These are “medical devices” just about everywhere.
That means they need testing, approval, and certification in one specific configuration.
Hacking or modding the hardware/software would require going through that whole process again in order to comply with the requirement for your doctor to keep monitoring it’s usage.
Obviously that doesn’t work for a one-off hack/mod.
It would probably be on the pretty dark side of the grey-area to show off mods and/or encourage others to do them.
I’m not saying I agree with this. Just why it happens.
That said, medical devices are FAR MORE than the sum of their parts.
A CPAP isn’t just an air pump anymore than an artificial heart is not simply a fluid pump.
Innovation and experimentation is a good thing.
But some things should be outside the realm of a garage hack.
I’d like to mention “OSCAR, the Open Source CPAP Analysis Reporter”. It reads the logged data from sd card from a CPAP machine. It enables the user to store, view and analyze this data locally. It generates graphs and statistics.
Oh, Lord, yes.
If your machine is supported, then OSCAR is an enormous help in understanding what goes on at night and how you can improve things.
https://www.sleepfiles.com/OSCAR/
An alternative is SleepHQ.
https://www.sleephq.com/
SleepHQ is an online service. It isn’t as detailed as OSCAR, but it makes it easier to share with someone for help in analysing your data.
“Machines typically deliver in the range of 4 to 20 cm H2O”
didn’t you mean cmHg ??
1cm H₂O is about 0.98 mbar. Apparently they still use this unit in hospitals.
Which is why my German doctor refers to millibar (metric) instead of using the squirrelly cmH2O unit.
Centimeter of water is the unit used in CPAP.
https://en.wikipedia.org/wiki/Centimetre_or_millimetre_of_water
I have sleep apnea. I received a machine and send it back after 2 months. I tried it every single night. It made falling asleep even more difficult and it kept waking me up. I never had any issues staying awake during the day. I’m always a bit tired but that’s it. But when trying the machine, I got into several sitautions where I almost had a major car accident because I was so tired that I kept misisng parts. Was driving and suddenly I was somewhere further down the road and a part was just missing. It messed with my job, it made it almost impossible to think. It’s a huge mess. It made all my problems so much worse. I could never get an actual night sleep with the cpap. I send it back. My “solution” which isn’t a solution at all, I know, is to have high stiff pillow. I put my head on the edge of the pillow so that half the head is on it and my face is pointing downwards. I curl up in my blanket and I can get a decent night sleep like that. It’s far from perfect and I’m trying to loose weight. I rarely drink.
And don’t forget, that the lack of oxygen can lead to heartgrowth and arrhythmia, which is in turn often misdiagnosed / mistreated.
If you have heart problems and some years of unsuccessfull treatment history, please go visit a sleep laboratory.
Been on CPAP for 30 Years. My transition was easy having been an avid SCUBA diver, wearing the mask was a non-issue. Turned my life around! Oh… on little tip. I keep a silver coin (old 1$) in my CPAP water tank. especially when traveling. I find that the silver keeps the Crud to zero, even if I have to resort to tap water for a night or two.
Neat
I recently got curious about how these worked and so I looked up Resmed patents to see how these work.
U.S. Patents No. 5,148,802 and 5,245,995
Also see EP1488743A2.
The machine can distinguish central apneas from obstructive by looking at the airflow pattern over the time of a breath. Obstructive apnea starts then drops off suddenly. This shows up in some of the drawings.
Technical term – Patency or patent = open or not obstructed.
There are two sensors – one mask pressure transducer and a differential pressure transducer for flow.
Technical term – Obstruction Index and Shape factor = Index of the state of the airway.
Approximately 5 seconds into the apnea a 2 Hz, 1 cm H2O pressure oscillation is induced (applied) by the pump for 6 seconds. Then the affect on flow is measured that can determine if the airway is open or not. Modulated pressure output. It’s a network analyzer for your airway!!!
I thought the feedback loop for control was interesting. The inner most loop of pressure and motor speed is analog, not digital. Then there are a few outer digital loops for other controls. It’s shown in one of the patents.
They could possibly detect your heart beat. Cardiogenic Airflow – observed airflow with each beat of the heart is of the order of 0.02 to 0.1 l/sec.
I’ve been on CPAP and now BiPAP for 20 years now, all Resmed. My first three nights were hell: I would thrash about until I pulled the machine to the floor. Third night… I knocked off a panel n the side. Trip pot and a display. Turned the pot and got a bigger number plus more air!
My 4th night I finally got my good night sleep.
Today you can’t use a heat code to up your air but the algorithms are much better. Time was I had to leave the auto shutoff disabled least the machine shut down.
I’m so acclimated to this I can’t fall asleep with out it.
I’ve been using one for years..fairly recently got the air sense 11.
I’m pretty sure the CPAP was a byproduct of CIA research on “enhanced interrogation methods”, i.e. torture.
I’ve been licensed to apply these to patients for 15 years. The math for determining what numbers to use is quite fun and rarely discussed. Hope the author gives it a whirl. There’s a LOT of arguments of how to set the numbers the patients use