Humans have lots of basic requirements that need to be met in order to stay alive. Food is a necessary one, though it’s possible to go without for great stretches of time. Water is more important, with survival becoming difficult beyond a few days in its absence. Most of all, though, we crave oxygen. Without an air supply, death arrives in mere minutes.
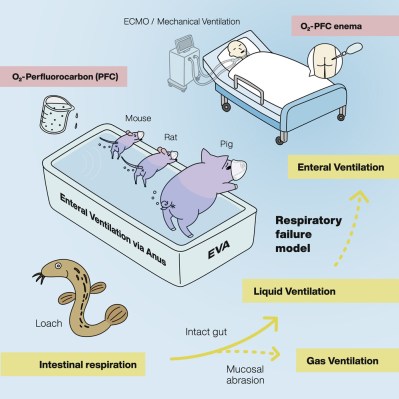
The importance of oxygen is why airway management is such a key part of emergency medicine. It can be particularly challenging in cases where there is significant trauma to the head, neck, or surrounding areas. In these cases, new research suggests there may be an alternative route to oxygenating the body—through the rear.
When Nothing Else Works
Most of us are familiar with the usual route of human respiration. We take in air through the mouth and nose, and it passes through the windpipe and into the lungs, where oxygen diffuses into the blood. When everything in the body is functional, this system works well. However, when things go wrong, it can suddenly become very difficult to keep a body alive.
Head or neck injuries can block the airway entirely, or infections can fill the lungs with fluid, preventing the transfer of oxygen to the blood. Supportive ventilation methods can help, but can often damage the lungs themselves while in use. When the lungs themselves cease to function at all, often the only real option is the use of a technique called extracorporeal membrane oxygenation, or ECMO. This is where complicated machinery is used to manually oxygenate the blood outside the body. It’s a complex method that can result in major complications, and comes with a wide range of potential side effects, some of which can be fatal.
In these life-or-death situations, it would be desirable to have an alternative oxygenation technique that could be used when the lungs or airway are badly compromised. New research has suggested that enteral ventilation could be just the ticket. It’s a rather out of the box method, involving the use of a special oxygen-carrying liquid called perfluorodecalin. By administering this fluid rectally, it may be possible to deliver oxygen to a patient without having to rely on the function of the lungs themselves.
As you might guess by the name, perfluorodecalin is a flurocarbon. Its molecules are made up of 10 carbon and 18 fluorine atoms, and it exists as a liquid at room temperature. It’s considered chemically and biologically inert, which is key to its use in a medical context. Beyond that, it’s capable of dissolving a great deal of oxygen, with 100 mL of perfluorodecalin able to dissolve 49 mL of oxygen at a temperature of 25 C. The fluid can also carry carbon dioxide, too. Historically, it’s been used as a method to supply oxygen to specific areas of the body in a topical application, and also used as a way to preserve organs or other tissues in an oxygen-rich environment.
Thus far, research remains at an early stage. Initial testing focused on supplying a rectal dose of non-oxygenated perfluorodecalin of 25 to 1,500 mL for up to 60 minutes, at which point patients would excrete the fluid on their own terms. Patients had their vital signs monitored and were studied for any possible adverse effects. The study found that only mild side effects occurred, specifically involving abdominal bloating and pain at higher levels which resolved without further intervention after the procedure was completed. No perfluorodecalin or related compounds were detected in the bloodstream in the immediate aftermath.
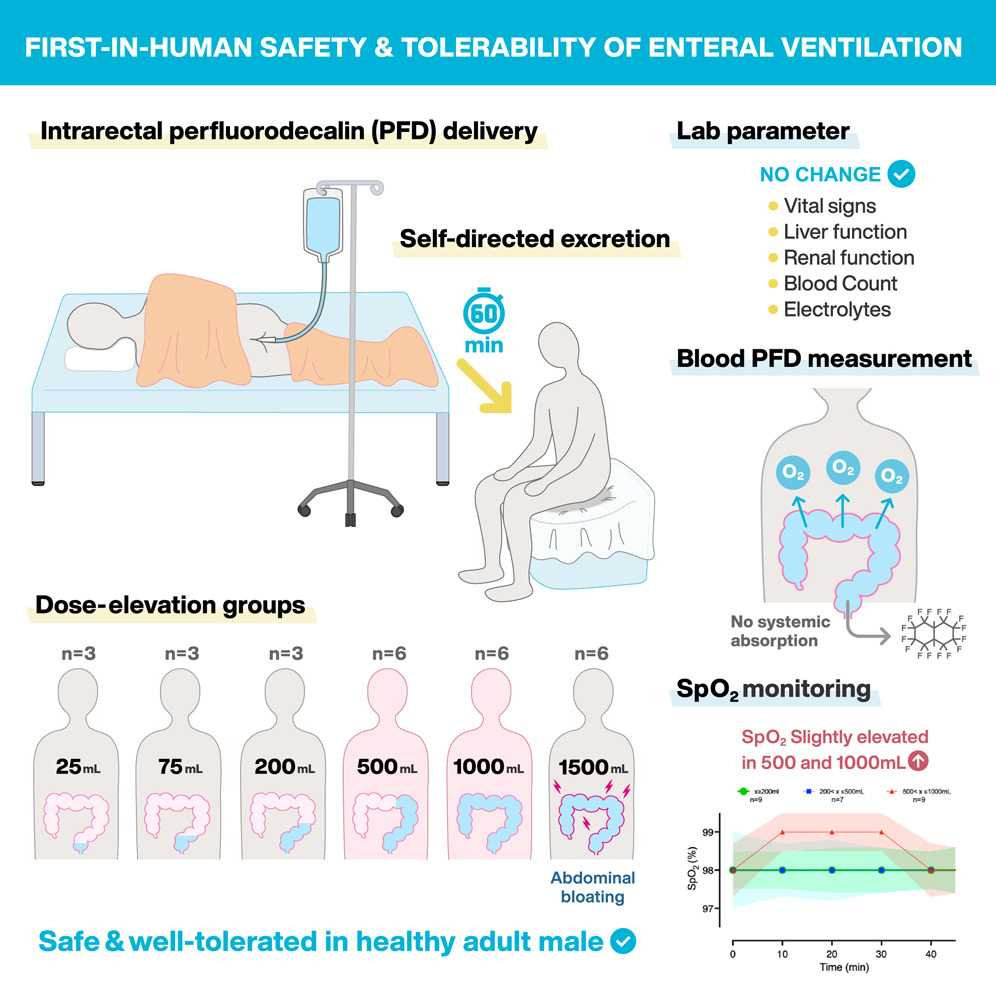
The first stage of clinical testing was focused on establishing safety profiles rather than outright testing the efficacy of rectal oxygenation. Nonetheless, even in testing with non-oxygenated perfluorodecalin, the study showed a “modest increase” in oxygen saturation in patients dosed with higher amounts of the fluid (500 mL and 1000 mL). This is a positive sign that this could be a viable route for oxygenation, but more research will be needed to verify the findings and develop the technique into something that could have actual clinical applications. That can be a particularly slow process due to the extensive safety requirements of new medical treatments, but such regulations exist for good reason.
First Rodeos And All That

It’s not the first time that physicians have explored alternate methods of delivering oxygen to the body. Other methods of liquid ventilation have been developed, albeit with a focus on delivering oxygen-rich liquids to the lungs themselves. The aim is generally to avoid the lung damage that is often caused by traditional positive-pressure ventilation systems, which can be particularly harmful to patients who are already badly unwell. Similarly, these methods typically use oxygen-rich flurocarbons to do the job. While there have been some promising studies, ultimately the technique remains experimental and challenging to implement.
Enteral ventilation has one major benefit over liquid ventilation using the lungs, precisely because it doesn’t involve the lungs at all. The body’s main airway can remain entirely unobstructed during such a treatment, and does not have to be filled with fluids or tubes that could cause damage on their own. In cases where the airway or lungs are badly damaged or compromised, these techniques could potentially help where liquid ventilation via the lungs would simply not be possible. There can be immediate risks in delivering any kind of liquid to a patient’s lungs, particularly if the transition to liquid breathing doesn’t go to plan. The same simply isn’t true of doing so via the enteral pathway, as the regular airway remains untouched and as functional as it ever was.
As it stands, you’re unlikely to be breathing via the rectum any time soon. However, some years down the line, your local emergency room or ICU might just have another route to administer oxygen when all the standard methods fail. It might be weird and unconventional, but it could help save lives.














I’ve heard of blowing smoke up your rear but this is new and seems practical unlike the old smoke method was was a sham treatment.
marijuana suppositories.
why not, the stuff already smells like someone lit a dog turd on fire!
Get better buds.
It should smell like skunk.
Why does it feel like that AI-generated article of rat with giant penis?
Just what I was thinking. Apparently a “loach” is a real thing. Maybe they used AI to make the artwork and touched it up by hand.
If they start using that on a regular basis, I’m going DNR.
I don’t mean to sound cold, but when my arse starts looking like a better place than my lungs for O2 transfer, I think it’s simply time for me to pack it up and go.
I suspect the intention would be it would be a short term option.
Never mind the need to clear our the colon before hand.
All this study showed was that the carrier wasn’t absorbed not that it was an effective way to deliver oxygen.
That said having a way to temporary replace the lungs would be incredibly useful even if only for 6 hours. And avoid ECMO.
Notorious side effects of this method are: bruises on hands, foggy mind, erratic speech, and weird hair coloration.
Why is this 404media.com content rebroadcast here?
Relevance to hacking?
I’m sure there’s a bad joke about backdoor pen testing there somewhere.
It feels a little early for April first.
I guess it can’t be any worse than secret service divers filling their lungs with an oxygenation liquid.
Oxygenated fluorocarbons were a space-research technology to enable high-G tolerance, although mostly only tried on mice. It was explored for deep sea diving in situations where hardsuits could not be used, but it turned out to be too fiddly for the gain (you can almost always get a free-swim hardsuit easier than you can get set up for fluorinert-based diving.
It’s a breathing hack.
Not all hacking involves hardware or software – that’s why we have bio-hacking.
Given that some (brave and/or foolhardy) folks actually experiment on themselves in similar ways, I’d say that a story about rectal oxygenation is right at home here on Hackaday. Even if some readers find it to be a pain in the butt…
Except there was no hack. They just put some liquid up people’s butts and saw that it came out.
Felching?
Nothing good ever comes from looking something up on urban dictionary.
Before looking that up, get drunk just short of blackout and poor large strong drink.
That way after you look it up, you have a chance of getting to ‘not putting down long term memory’ before it commits.
Seems to me that continuously infusing through a long catheter high in the colon and continuously draining though another catheter placed near the exit would obviate the need for “self-directed excretion.” Instead of ECMO (Extra-Corporeal Membrane Oxygenation) we would have ICCO (Intra-Corporeal Colonic Oxygenation). Pronounced “icky.” And you would not become hypoxic while sitting on the toilet.
That seems like a great idea! Continuously re-oxygenating the fluid as it circulates would allow the patient to rest more fully, possibly speeding up the healing of the lungs. And the continuous circulation might increase the speed of oxygen uptake, making the process more effective and efficient.
The study utilized “self-directed excretion” because the aim was to establish that the fluid is safe when introduced into the anus and colon, not actually perform ECMO. That being said, “icky” is a winner albeit not quite the obvious way to pronounce “ICCO”.
Maybe a peritoneal dialysis could be adapted for oxygen delivery, too? It’s a semi-permeable membrane that is well supplied with blood, so it should work.
Didn’t some guy die recently from sticking an air compressor hose up his bum..
Too much of anything can kill you.
as per Galen, the dose makes the poison
That was Paracelcus who said that.
I am sure Galen said it too
im not surprised. pr0n sites have entire categories for air/liquid inflation.
its also been known to be used medically for a “virtual colonoscopy”, though that’s a lot less fun.
That’s one of the results of saline solution injection: https://edramatica.com/images/d/d7/Big_Bag.gif
Ugh, that cannot be unseen!
Compressed air safety training:
More than once, someone has been killed by a jackass firing high pressure air at their butthole.
They don’t have to put anything up the butt, just spray compressed air at the butt and roll a 20.
Also oral sex safety training:
Never inflate a ‘giner by giving ‘blow job’.
It can kill her.
Tell them spacemen to leave me alone!
I’m tired of being adbuckted…I done been reamed out by them and their probes…
If it’s good enough for a Cray T90 it’s good enough for me.
If it’s good enough for sea turtles.
at least its a new avenue for strangulation bondage. controlled hypoxia as a sexual fettish. i feel like this could have saved david caradine’s life.
I think he had too many hangups for it to work out.
I don’t think this is appropriate to post here, there are children and teenagers reading here!
GTF out.
If they get it, they are old enough.
Also not our problem, internet was built by adults for adults (for porn).
Parents letting their spawn loose on unfiltered net is nobodies problem but theirs.
If someone would tell me this with a straight face at a party I would doubt if tall tale or truth.
This research seems like an igNobel Prize candidate.
Nah, this would be really handy in the ER, just messy as hell I’d imagine. But if the alternative is “I just couldn’t get an airway on this kid” then who cares. The patient would likely not have any problems with this, given the other option.
I can see this as the next big Medical Spa treatment, you can have a fish semen facial treatment and an oxygen enema.
Can this be used at an oxygen Bar? Will football players be using this? Would this be considered doping?
People are going to try to make money off it outside of strictly medical procedures, but I am not sure how outside of the Medical Spa Treatment.
“Mooooon river…”
Some people consume vodka via anus to bypass breathalyzer
Does not work. Whichever way you get alcohol in your blood stream, it will show in breathalyzer test.
“However, some years down the line, your local emergency room or ICU might just have another route to administer oxygen when all the standard methods fail.”
I need to ask McCoy where he keeps the tri-ox injector.
Three things, one is that there is research showing that it is valid way to rehydrate using salt water with a sea water enema, and it has been used in emergencies; during a colonoscopy the techs inflate your bowels with CO2 since it is readily absorbed into your system and thrown off through respiration, and it is easier on the body than having to fart for several minutes; however THE SIRENS OF TITAN was SUPPOSED to just be FICTION
(The Martian army relied on oxygen suppositories to operate on unsealed areas on Mars)
Fun fact.
Most fart gas is absorbed by the colon and breathed out via the lungs.
The epic fart at the end of a colonoscopy is the best part.
I’ll be dead before farts stop being funny.
‘Promising rials ..’ is the capTion of The firsT picTure of The arTicle. Perhaps a leTTer is missing?
If they really wanted to do something, a nasal feeding tube placed post-pyloric (past the outlet of the stomach) could just dump that liquid into the GI system from the top (South Park aside…) you know, the normal direction for stuff to move in the body, and it would likewise exit via the normal route. Just like anyone that has ever had a GI procedure and had to do the prep. I’m guessing that fluid is crazy expensive but eh, so is all health care in the US. Re use, I’ll leave that to the reader to decide but a “fecal transplant” is a real thing so… it is not unheard of.
.
I did read the primary literature, and while “promising” and all that other media stuff is technically correct, a 10-20mmHg increase in pO2 in the blood for a few minutes via the butt isn’t what I’d call clinically relevant. For reference, normal pO2 on room air is about 100 mmHg, and with a simple facemask you can push that all the way up to like 500+ mmHg but the rub is that you aren’t increasing the total amount of oxygen in the blood by very much at all- the hemoglobin is nearly entirely saturated already and that’s what is carrying the O2 (see: alveolar gas equation). It is only increasing the tiny bit dissolved in the plasma itself. That’s with normal lungs though. Intubation and ventilation can do better, but when the lungs are that messed up it’s hard. ECMO for purely respiratory failure is pretty uncommon indication, but the type used for that is VV ECMO and doesn’t have a lot of the risks associated with “regular” ECMO. This is already too long sorry. It is a huge topic.
Eh self-reply.
About the only clinical thing I could think of where this would maybe be helpful is an in-hospital choking event where it just maybe would give you long enough to do a bronch and pull out the obstruction, or maybe maybe an acutely recognized pulmonary saddle embolus (look it up.. it is bad) to give you enough time to wheel down to the cath lab. Even for those though, going from zero oxygen to 10-20 mmHg oxygen in the blood… worth a try I guess.
I disagree about PE. A saddle embolism causes no flow through the system, so absorb all the oxygen you want. It can’t get anywhere. Saddle PE needs venous to arterial ECMO. The pump in the machine is what would make it work physiologically in that situation.
First off I super-qualified that statement with “maybe maybe” and second off, a humungous saddle PE yeah. You are done right there. No flow. But you can also have one stuck at the bifuration of the pulmonary trunk that doesn’t entirely occlude one or both pulmonary arteries so there is some flow and yeah, I’ve personally treated a patient or two that made it to the cath lab nominally alive after a big PE so… like I said above, if you are gonna die anyway , maybe maybe ass-oxygen could help. I cannot remembver if they got TPA or heparin or what, it was ages ago in another life. But I stand by what I said… Maybe. Maybe.
Sounds like fancy doctor words for ‘vapor locked heart’.
Not sure a heart worth of gas circulating is an improvement.
Worth noting this was just a trial with non-oxygenated fluid to test tolerance. Hence the low SPo2 increase.
Um, no.
…
“PFD bubbled with pure O2 for 30 minutes was administered into the rectum of pigs” (caption figure 3)
and .
“O2-loaded PFD was thus prepared (1L bulbbling per minute for 45 minutes; Figure 2A”
That’s right from the paper linked right there in the article: Med 2, 773-783, June 11, 2021
Was it the same liquid they filled the lungs with in the The Abyss movie?
According to Wikipedia, both are perfluorinated compounds but not the same. The study used perfluorodecalin while the Abyss used Fluorinert (perflurohexane or perfluorotripentylamine.)
I am Cornholio! I need Fluorinert for my bunghole!
This could be great for politicians. They can breathe through their ass since they already talk out of it. Multitasking!
I used to donate blood plasma and the cool half liter shot of isotonic saline at the end was quite refreshing in Summer. Maybe it could become a liquid cooling solution?
Not a single comment on the “Respiratory Failure Model” image? Two things:
a) makes the whole thing smell fake. Soaking the rear end of a mouse, rat, pig in a vat of PFC … I mean, if they had showed the animals having an enema at least that might smack of ‘real’; b
b) if you have to kill another living thing and mask the reality by calling the living thing a “model” then are you really doing “science”? Surely a “science” could find a better way to confirm a hypothesis not just the easiest or most convenient way?
This isn’t that much of a breaking research. All they were doing is showing that an existing common medically-available fluorinated compound was also safe for this other use. It smells more like a student project than major research, because the compound in question is already generally recognized as safe for medical-environment use. All of the graphics are familiar; they’re standard clip art in one of the commonly available report/paper writing environments.
The main difference with past experiments was that the previous experiments used fluorinert; the difference is mainly regulatory and certification; an existing medical-use compount has a lower barrier to experimentation.
I thought this was shown a few years back but without the need for a working fluid.
Straight gaseous oxygen works, but not as well, and has greater potential for side effects (the membranes are kind of delicate and don’t always respond well to contact with gaseous oxygen).
AI Slop papers were rarer in 2021 and this 2025 paper seems to follow their earlier 2021 https://www.cell.com/med/fulltext/S2666-6340(21)00153-7 and 2023 papers https://www.cell.com/iscience/fulltext/S2589-0042(23)00219-5
“Enteral liquid ventilation oxygenates a hypoxic pig model”
“Mammalian enteral ventilation ameliorates respiratory failure”
In this 2025 paper phase one paper they have furthered the 2021 and 2023 papers by squirting up to a litre of the stuff into 27 humans, to see how they can handle it.
And the answer is ok outside obdominally bloated, which was self resolving.
A box covered with a sheet and… That’s a toilet?
Better to use gentle suction in the bed, they might not be very mobile.
Please try all other ways to save me first.