Opioid overdose-related deaths have unfortunately been increasing over the last few decades, with the COVID-19 pandemic exacerbating this public health crisis even further. As a result, many scientists, healthcare professionals, and government officials have been working tirelessly to end this deadly epidemic. Researchers at the University of Washington are one such group and have recently unveiled a wearable to both detect opioid overdose and deliver an antidote, in real-time, restoring normal bodily function.
As the researchers describe in their paper, opioid overdose causes respiratory rate depression which will lead to hypoxia (insufficient oxygen in the blood) and ultimately death. Fortunately, opioid overdose can be readily reversed using naloxone, a compound that binds to receptors in the brain, outcompeting the opiates themselves, and restoring normal breathing. Unfortunately, if someone is overdosing, they are unable to self-administer the antidote and with many opioid overdoses occurring when the victim is alone (51.8%), it is necessary to develop an automated system to deliver the antidote when an overdose is detected.
The researchers begin by describing their process for measuring respiration, of which there are several options. You could use photoplethysmography in much of the same way we measure heart rate. Or you could measure the changing impedance of the chest cavity during breathing or even use an intraoral sensor that measures airflow in the mouth. Instead, the researchers opt to measure respiration by attaching accelerometers to the patient’s abdomen and measuring the movement of the abdominal cavity during breathing. They admit their technique becomes problematic when the patient is not stationary, but argue that in the case of a drug overdose, the patient is likely to be immobilized and the device would be able to measure respiration with ease. They tested their device across dozens of healthy, human volunteers, and even some opiate users themselves, and showed their technique had good agreement with a reference respiratory belt placed around the volunteers’ chests.
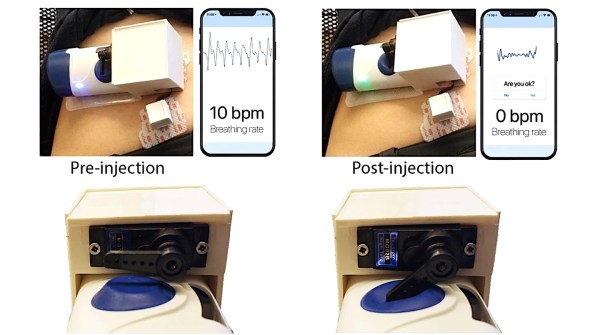
The cool part about this paper is that they demonstrated a “closed-loop” feedback system in which their device measured respiration, detected cessation in breathing (indicating an overdose), and delivered the antidote. To deliver naloxone, they leveraged an existing, commercially-available drug delivery system that requires a user to manually activate the device by pressing a button. They hacked the device a bit such that the trigger could be actuated using a servo motor properly positioned to depress the button when an opioid overdose is detected. They simulated an overdose by asking the healthy, human volunteers to hold their breath for a period greater than 15 seconds. They were able to successfully deliver the antidote to 100% of their volunteer group, indicating the device could potentially work in real-world settings.
Now, the form factor of the device undoubtedly needs to improve in order to deploy this device into the field, but we imagine those are improvements are underway and patients have shown willingness to wear such devices already. Also, there’s still a bit of a question of whether or not accelerometer-based breathing detection is optimal since some drug overdoses cause seizures. Nevertheless, this is an important step in combating the alarming rise in opioid overdose-related deaths and we hope to see many more advances in patient monitoring technologies in this field.