Join us on Wednesday, October 16 at noon Pacific for the Hacking Diabetes Hack Chat with Dana Lewis!
When your child is newly diagnosed with Type 1 diabetes (T1D), everyone is quick to point out, “It’s a great time to be a diabetic.” To some degree, that’s true; thanks to genetically engineered insulin, more frequent or even continuous glucose monitoring (CGM), and insulin infusion pumps, diabetics can now avoid many of the truly terrifying complications of a life lived with chronically elevated blood glucose, like heart disease, kidney failure, blindness, and amputations.
Despite these advances, managing T1D can be an overwhelming task. Every bite of food, every minute of exercise, and every metabolic challenge has to be factored into the calculations for how much insulin to take. Diabetics learn to “think like a pancreas,” but it’s never good enough, and the long-promised day of a true artificial pancreas always seems to remain five years in the future.
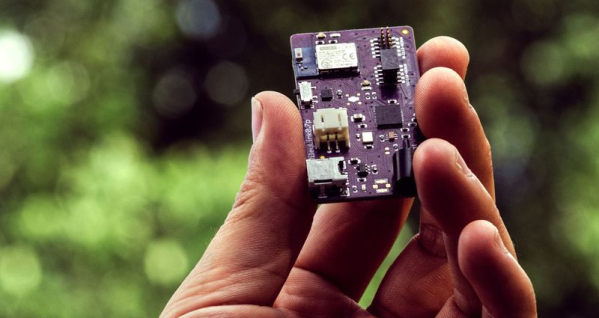
Dana Lewis is one diabetic who decided not to wait. After realizing that she could get data from her CGM, she built a system to allow friends and family to monitor her blood glucose readings remotely. With the addition of a Raspberry Pi and some predictive algorithms, she later built an open-source artificial pancreas, which she uses every day. And now she’s helping others take control of their diabetes and build their own devices through OpenAPS.org.
Join us on the Hack Chat as Dana drops by to discuss OpenAPS and her artificial pancreas. We’ll find out what her background is – spoiler alert: she wasn’t a hacker when she started this – what challenges she faced, the state of the OpenAPS project, and where she sees the artificial pancreas going.
 Our Hack Chats are live community events in the Hackaday.io Hack Chat group messaging. This week we’ll be sitting down on Wednesday, October 16 at 12:00 PM Pacific time. If time zones have got you down, we have a handy time zone converter.
Our Hack Chats are live community events in the Hackaday.io Hack Chat group messaging. This week we’ll be sitting down on Wednesday, October 16 at 12:00 PM Pacific time. If time zones have got you down, we have a handy time zone converter.
Click that speech bubble to the right, and you’ll be taken directly to the Hack Chat group on Hackaday.io. You don’t have to wait until Wednesday; join whenever you want and you can see what the community is talking about.
[Dana Lewis image source: GeekWire]