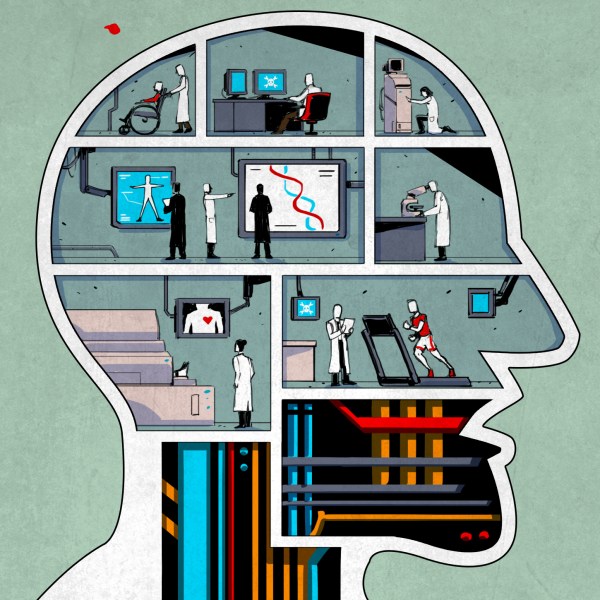
Everyone starts their day with a routine, and like most people these days, mine starts by checking my phone. But where most people look for the weather update, local traffic, or even check Twitter or Facebook, I use my phone to peer an inch inside my daughter’s abdomen. There, a tiny electrochemical sensor continuously samples the fluid between her cells, measuring the concentration of glucose so that we can control the amount of insulin she’s receiving through her insulin pump.
Type 1 diabetes is a nasty disease, usually sprung on the victim early in life and making every day a series of medical procedures – calculating the correct amount of insulin to use for each morsel of food consumed, dealing with the inevitable high and low blood glucose readings, and pinprick after pinprick to test the blood. Continuous glucose monitoring (CGM) has been a godsend to us and millions of diabetic families, as it gives us the freedom to let our kids be kids and go on sleepovers and have one more slice of pizza without turning it into a major project. Plus, good control of blood glucose means less chance of the dire consequences of diabetes later in life, like blindness, heart disease, and amputations. And I have to say I think it’s pretty neat that I have telemetry on my child; we like to call her our “cyborg kid.”
But for all the benefits of CGM, it’s not without its downsides. It’s wickedly expensive in terms of consumables and electronics, it requires an invasive procedure to place sensors, and even in this age of tiny electronics, it’s still comparatively bulky. It seems like we should be a lot further along with the technology than we are, but as it turns out, CGM is actually pretty hard to do, and there are some pretty solid reasons why the technology seems stuck.
Continue reading “Why Is Continuous Glucose Monitoring So Hard?”