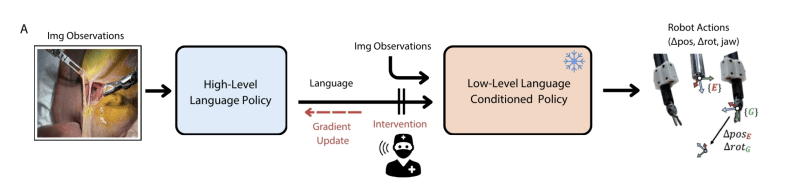
Taking a look inside the human body has never been easier — just swallow a camera in the shape of a pill. However, what is not quite as easy is retrieving a piece of whatever you’re viewing. This is exactly what researchers from HIT Shenzhen have attempted to solve with their magnetic capsule bot.
When traditional procedures want to take a sample somewhere in the intestinal tract they generally require somewhat invasive procedures sticking something up…well you know. With this pill, robot magnetic control allows physicians to choose exactly where and when to take a sample, all without shoving unpleasant objects into…again you know.
A magnetic field is generated to open the capsule and suck liquids inside. This traps a sample that can be retrieved through later bowel movements. The technology hasn’t been tested on a living patient yet, but but animal trials are planned for the foreseeable future.
Check out the fine details with the paper itself here. Biomedical engineering is always an interesting topic with so much potential for more hacking. We at Hackaday are no strangers to this wonderful world of bodily hacks.