Genetic defects are exceedingly common, which is not surprising considering just how many cells make up our bodies, including our reproductive cells. While most of these defects have no or only minor effects, some range from serious to fatal. One of these defects is in the CPS1 gene, with those affected facing a shortened lifespan along with intensive treatments and a liver transplant as the only real solution. This may now be changing, after the first successful genetic treatment of an infant with CPS1 deficiency.
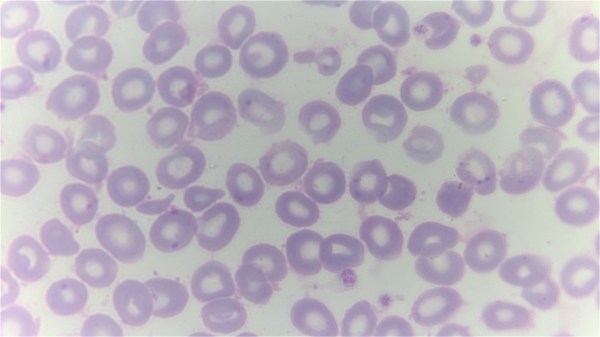
Carbamoyl phosphate synthetase I (CPS1) is an enzyme that is crucial for breaking down the ammonia that is formed when proteins are broken down. If the body doesn’t produce enough of this enzyme in the liver, ammonia will accumulate in the blood, eventually reaching levels where it will affect primarily the nervous system. As an autosomal recessive metabolic disorder it requires both parents to be carriers, with the severity depending on the exact mutation.
In the case of the affected infant, KJ Muldoon, the CPS1 deficiency was severe with only a low-protein diet and ammonia-lowering (nitrogen scavenging) medication keeping the child alive while a search for a donor liver had begun. It is in this context that in a few months time a CRISPR-Cas9 therapy was developed that so far appears to fixing the faulty genes in the liver cells.
Continue reading “Fixing A Fatal Genetic Defect In Babies With A Bit Of Genetic Modification”