If you’re feeling underwhelmed by yet another smartwatch announcement, then researchers at the University of Maryland may have just the wearable for you. Instead of just tracking your movement from one spot, Calico winds around you like a cartoon sidekick.
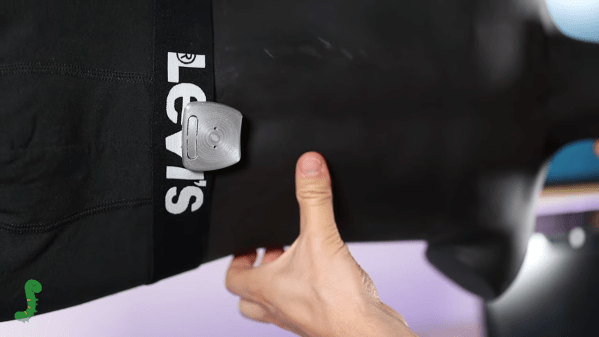
Using a “railway system,”(PDF) the Calico can travel around a garment to get better telemetry than if it were shackled to a wrist. By moving around the body, the robot can track exercise, teach dance moves, or take up-close heart measurements. Tracks can be magnetically linked across garments, and Calico can use different movement patterns to communicate information to the user.
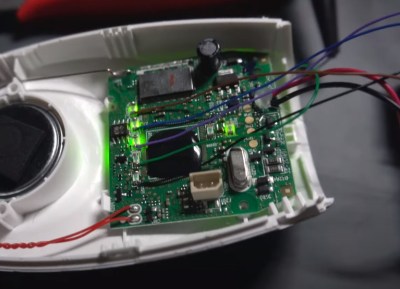
This two-wheeled robot that rides the rails is built around a custom PCB with a MDBT42Q microcontroller for a brain which lets it communicate with a smartphone over Bluetooth Low Energy. Location is monitored by small magnets embedded in the silicone and plastic living hinge track, and it can use location as a way to provide “ambient visual feedback.”
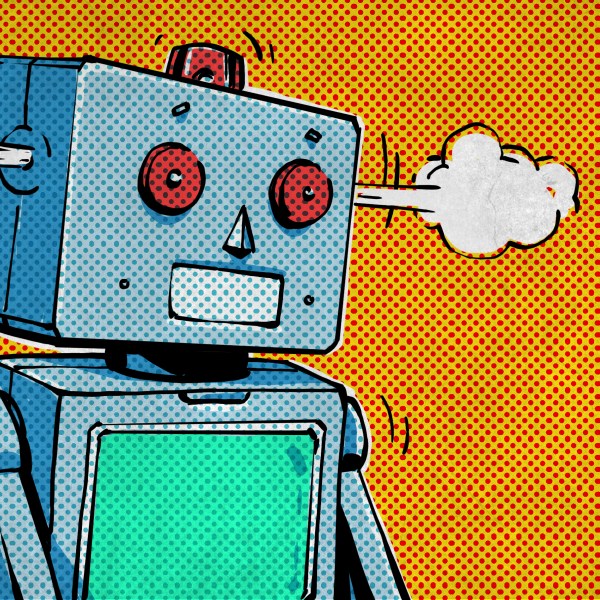
The researchers even designed a friendly cover for the robot with googly eyes so that the device feels more personable. We think animated wearables could really take off since everyone loves cute animal companions, assuming they don’t fall into the uncanny valley.
If you love unusual wearables as much as we do, be sure to check out Wearable Sensors on Your Skin and the Wearable Cone of Silence.







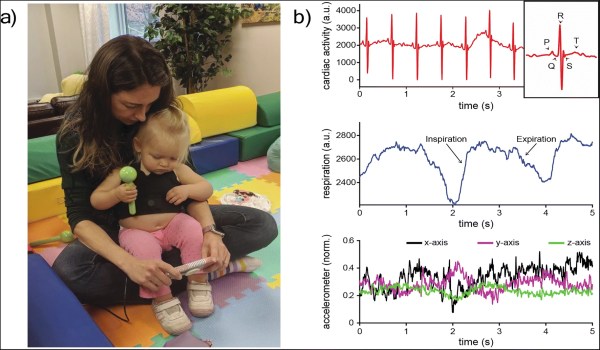
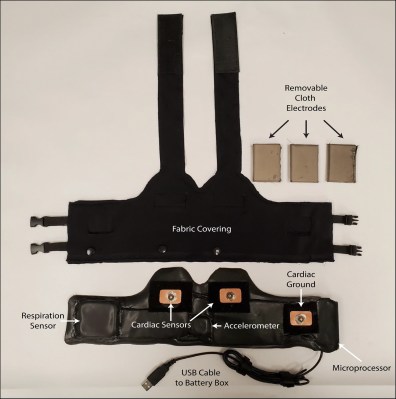 Their device includes a number of components we’ve seen already. There is an HC-05 Bluetooth module,
Their device includes a number of components we’ve seen already. There is an HC-05 Bluetooth module,