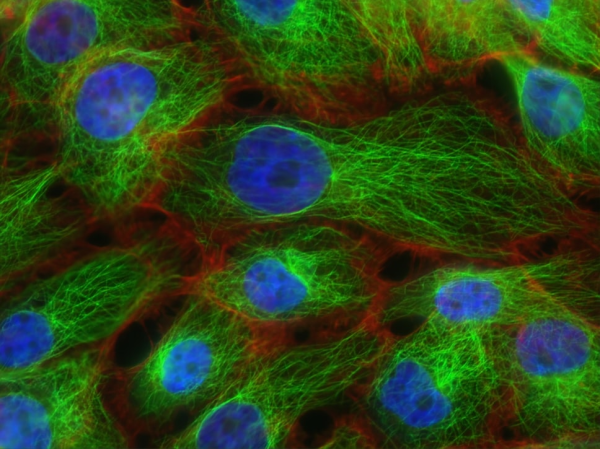
As areas of uncontrolled cell growth, cancerous growth form a major problem for a multi-celled organism like us humans. Thus before they can begin to affect our long-term prospects of a continued existence, eradicating these cells-gone-wrong is essential. Unfortunately, doing so without affecting healthy cells significantly is tough. Treatments such as chemotherapy are correspondingly rough on the body, while radiation therapy is a lot more directed. Perhaps one of the more fascinating treatments involves ultrasound, with the IEEE Spectrum magazine recently covering one company providing histotripsy equipment.

Ultrasound has found many applications in the medical field far beyond imaging, with therapeutic ultrasound by itself covering a variety of methods to perform actions within the body without breaking the skin. By using high-energy ultrasound, everything from kidney stones to fat cells and cancerous cells can be accurately targeted and destroyed. For liver tumors the application of so-called histotropsy has become quite common, allowing certain types of tumors to be ablated non-invasively after which the body can handle the clean-up.
Histotropsy is a form of high-intensify focused ultrasound (HIFU) that uses either continuous or pulsed waves to achieve the desired effect, with the HIFU transducer equipped with an acoustic lens to establish a focal point. In the case of histotripsy cavitation is induced at this focal point that ends up destroying the local tissue. Beyond liver tumors the expectation is that other tumors will soon be treated in a similar manner, which could be good news for especially solid tumors.
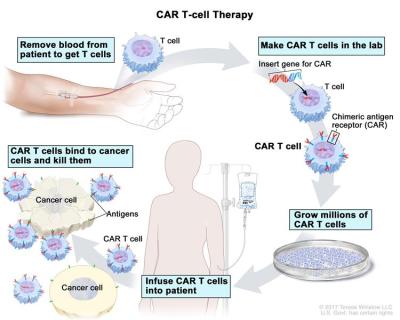
Along with new approaches like CAR T cell immunotherapy, the prospects for cancer becoming a very treatable set of diseases would seem to be brighter than ever.